Uroxatral
Cheap generic uroxatral canada
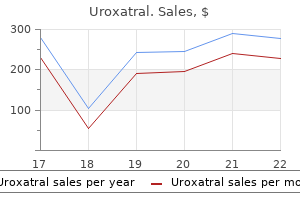
Severe micrognathia is associated with polyhydramnios possibly because of the glossoptosis preventing swallowing prostate infection treatment buy cheap uroxatral on line. Severe micrognathia can be a neonatal emergency due to airway obstruction by the tongue in the small oral cavity. If prenatal diagnosis is made a pediatrician should be present in the delivery room and be prepared to intubate the infant. In general, about half are either lethal or require surgery and half are asymptomatic. Prevalence Cardiovascular abnormalities are found in 5-10 per 1, 000 live births and in about 30 per 1, 000 stillbirths. Etiology the etiology of heart defects is heterogeneous and probably depends on the interplay of multiple genetic and environmental factors, including maternal diabetes mellitus or collagen disease, exposure to drugs such as lithium, and viral infections such as rubella. Specific mutant gene defects and chromosomal abnormalities account for less than 5% of the patients. Heart defects are found in more than 90% of fetuses with trisomy 18 or 13, 50% of trisomy 21, and 40% of those with Turner syndrome, deletions or partial trisomies involving a variety of chromosomes. Recurrence When a previous sibling has had a congenital heart defect, in the absence of a known genetic syndrome, the risk of recurrence is about 2%, and with two affected siblings the risk is 10%. When the father is affected, the risk for the offspring is about 2% and if the mother is affected the risk is about 10%. Reliability of prenatal diagnosis Echocardiography has been successfully applied to the prenatal assessment of the fetal cardiac function and structure, and has led to the diagnosis of most cardiac abnormalities. However, the majority of such studies refer to the prenatal diagnosis of moderate to major defects in high-risk populations. Screening for cardiac abnormalities the main challenge in prenatal diagnosis is to identify the high-risk group for referral to specialist centers. The indications include congenital cardiac defects in one of the parents or previous pregnancies, maternal diabetes mellitus or ingestion of teratogenic drugs. However, more than 90% of fetuses with cardiac defects are from families without such risk factors. A higher sensitivity is achieved by examination of the four-chamber view of the heart at the routine 20-week scan; screening studies have reported the detection of about 30% of major cardiac defects. Recent evidence suggests that a higher sensitivity (more than 50%) can be achieved by referral for specialist echocardiography of patients with increased nuchal translucency at 10-14 weeks. These planes include the four-chamber, left and right chambers and great vessel views. Although it is convenient to refer to these standardized views for descriptive purposes, in practice it may be difficult to reproduce these exact sections, and the operator should be familiar with small variations of these planes. Complex cardiac anomalies are frequently associated with an abnormal disposition of the heart and extra-cardiac viscera. Fetal echocardiography should always include an assessment of topographic anatomy of the abdomen and chest. The left and right sides are assessed by determining the relative position of the head and spine. The visceral situs is then assessed by demonstrating the relative position of the stomach, hepatic vessels, abdominal aorta and inferior vena cava. The examination of the fetal heart begins with the assessment of the disposition of abdominal and thoracic organs, as an abnormal disposition is frequently associated with complex cardiac anomalies. A transverse section of the upper abdomen, the same used for the measurement of the abdominal circumference, allows to identify the position of the liver, stomach and great abdominal vessels. A transverse section of the thorax reveals the four-chamber view of the fetal heart. The heart is not mid-line but shifted to the left side of the chest, with the apex pointing to the left. The axis of the interventricular septum is about 45 to 20 to the left of the anteroposterior axis of the fetus. The examination of the fetal heart begins with the assessment of the disposition of abdominal and thoracic organs In the four chamber view the normal ventricles, atria, atrio-ventricular valves, ventricular and atrial septae, foramen ovale flap, and pulmonary venous connections can be identified. The thickness of the interventricular septum and of the free ventricular walls is the same. The foramen ovale flap is visible in the left atrium, beating toward the left side. The insertion of the tricuspid valve along the interventricular septum is more apical than the insertion of the mitral valve. The confluence of the pulmonary veins into the left atrium serves to identify it as such. Probably, about 90% of ultrasonographically detectable fetal cardiac defects demonstrate some abnormalities in this view. Normal Cardiac Axis Evaluation of the cardiac outflow tracts can be difficult, and at present it is not considered a part of the standard examination of fetal anatomy. However, we believe that it is important to attempt such an examination because this improves the detection of many abnormalities of the heart and great arteries. The outflow tracts and great arteries can be demonstrated by slight angulations of the transducer from the four-chamber view. By turning the transducer while keeping the left ventricle and the aorta in the same plane, one can obtain the left heart views, while the right heart views are obtained by moving the transducer cranially and tilting slightly in the direction of the left shoulder. The right heart views demonstrate the right ventricle and the right ventricular outflow tract. The main pulmonary artery originates from the anterior ventricle and trifurcates into a large vessel, the ductus going into the descending aorta, and two small vessels, the pulmonary arteries There are two arches in the fetus (aortic arch and curve of the ductus) and they should be distinguished. The brachiocephalic vessels originate from the aortic arch, while no vessels emanate from the ductus. Furthermore, the curve of the aortic arch is gentler than that of the ductus, which is slightly more angular. M-mode, which is not used routinely, is useful for the evaluation of abnormal cases. In M-mode ultrasound, one line of information only is continuously displayed: instead of a two dimensional scan of the heart, a recording of the variations of echoes along a single line is produced. Thus, M-mode is of little help in the analysis of the morphology of the heart but is useful in assessing motions and rhythms. Pulsed wave and color Doppler Color Doppler overlays a representation of flow velocity over a conventional gray scale image. Color Doppler is useful to assess normal anatomy and physiology, valvular regurgitation or stenosis, shunting and the orientation of flows. Pulsed wave Doppler is used to analyze the spectral shift (to assess the resistance in a vessel), to obtain flow velocities (how the resistance affects the flow), and flow predictions (to estimate the perfusion). Pulsed Doppler ultrasound, in combination with two-dimensional and M-mode sonography, has proved useful in the evaluation of both fetal dysrhythmias and structural anomalies. Pulsed Doppler can be useful in the detection and assessment of severity of valvar abnormalities (stenosis, insufficiency). Analysis of atrioventricular inflows, hepatic veins and inferior vena cava can also be used to assess cardiac rhythm. Primum atrial septal defect is the simplest form of the atrioventricular septal defects (see below). Secundum atrial septal defect, which are the most common, are usually isolated, but may be related to other cardiac lesions (such as mitral, pulmonary, tricuspid or aortic atresia) and are occasionally found as part of syndromes (including Holt-Oram syndrome in which there is hypo aplasia of the thumb and radius, triphalangeal thumb, abrachia, and phocomelia). Prevalence Secundum atrial septal defects, which represent about 10% of congenital heart defects, are found in about 1 per 3, 000 births. Diagnosis Although the in utero identification of secundum atrial septal defect has been reported, the diagnosis remains difficult because of the physiological presence of the foramen ovale and only unusually large defects can be recognized with certainty. Prognosis Atrial septal septal defects are not a cause of impairment of cardiac function in utero, as a large right-to-left shunt at the level of the atria is a physiological condition in the fetus. They are classified into perimembranous, inlet, trabecular or outlet defects depending on their location on the septum. Perimembranous defects (80%) involve the membranous septum below the aortic valve, but also extend to variable degrees into the adjacent portion of the septum. The inlet defects are on the inflow tract of the right ventricle and thus affect the implantation of the septal chordae of the tricuspid valve.
Syndromes
- Aloofness
- Bleeding
- Thickening and hardening of the skin on the legs and ankles (lipodermatosclerosis)
- Some infections
- Male pattern baldness
- Ovulation (the production and release of an egg from your ovary in the middle of your menstrual cycle)
- IVP - less utilized tests
Buy uroxatral 10mg without prescription
Tese characteristics are fully described by site of metastases prostate cancer life expectancy purchase cheap uroxatral line, resulting in bone distortion. The the patient, so the condition should be investigated as stretching of periosteum by tumor expansion, mechani probable osseous metastasis with bone pain. Pain is cytokines, which mediate osteoclastic bone destruction, usually bilateral when originating in the thoracic spine may activate pain receptors. Straight leg raising, coughing, row probably accounts for the observation that pain and local pressure can exaggerate the pain, while pain produced by tumors is often disproportionate to their may be relieved by sitting up or lying absolutely still. A secondary pain Weakness, sphincter impairment, and sensory loss are may be caused by reactive muscle spasm. Nerve root in uncommon at presentation, but they develop when ltration and the compression of nerves by the collapse the disease progresses in the compressive phase, and of osteolytic vertebrae are other sources of pain. As half of the calcium is albumin-bound, the total calcium Case study value should be adjusted for the albumin level to cor A female patient, aged 63 years, came to the pain clinic rectly evaluate the calcemic status. Renal function, in with vague aching pain in the lower back, which she has cluding urea and electrolytes, should be checked. Symp had for 3 months, accompanied by gnawing pain in the toms occur with calcium values exceeding 3 mmol/L, middle of her right thigh, particularly on standing up and their severity is correlated with higher values. Pain scoring by the patient dened the pain elderly and very ill patients, very slight increases of ion at rest as 4, and pain on walking as 6, on a 10-cm line. The patient has had radical left into the circulation secondary to an increased breast surgery due to breast cancer, followed up by radio bone resorption. Both urinary hy Pain may be vague or absent because osseous droxyproline/creatinine and calcium/creatinine metastasis may be painless. However, any vague pain ratio have been used to monitor the eects of in a patient with a history of treated cancer should be bisphosphonate treatment. Pain as vomiting, anorexia, constipation, weakness, de a symptom is present in about 50% of patients. The ve hydration, polyuria, mental disturbances, and most frequently involved sites are the vertebrae, pelvis, confusion. Gastrointestinal a period of weeks or months, becoming progressively symptoms are often mistaken for opioid eects or more severe. The pain usually is localized in a particular are potentiated by opioid-related symptoms, and area, such as the back and the lower third of the femur, neurological symptoms are often attributed to ce and is often felt at night or on weight bearing. Patients with a and integrity of the spinal cord, and allows dierentia myeloma presenting low values of serum osteo tion between traumatic, osteoporotic, or pathological calcin, a sensitive and specic marker of osteo fractures and compression without the need of invasive blastic activity, have advanced disease, extensive techniques, such as myelography. With conventional radiography plications including pain and hypercalcemia can then be a change of about 40% in bone density is required be alleviated. The most important is radiation therapy, or fore bone metastases may be identied, and small le the use of radionuclides. However, using a standard treatment regime delivering 60 Gy in the method is less sensitive for the detection of pure 30 fractions over 6 weeks with daily treatment sessions. Bone scan abnormalities are Radiotherapy should be the rst step in the manage not specic, and several benign conditions give rise to ment of metastatic bone pain. Scans may appear negative when an adjunct to orthopedic surgery to decrease the risk lesions are predominantly osteolytic, after radiother of skeletal complications. Radiotherapy is used for bone metas type of metastases and yield more sensitive results tases to relieve pain, prevent impending pathological than the previous methods. Currently, immediate-release forms of morphine, well as eects specically related to the irradiation eld, oxycodone, and hydromorphone are available for a fairly including skin lesions, gastrointestinal symptoms, my rapid onset of drug action. The best treatment for arations (morphine, oxycodone, or hydromorphone) are hypercalcemia due to cancer is treatment of the cancer eective in dosing every 12 or 24 hours, or sometimes itself. They are usually used after dose titration tients whose cancer is advanced or has not responded to dene the eective daily dose for baseline continu to treatment, management of hypercalcemia is some ous pain. Radionuclides Long-term use of opioids is associated with Radionuclides that are absorbed at areas of high bone physical dependence and (rarely) tolerance. Tolerance turnover have been assessed as potential therapies for is dened as a physiological phenomenon of progressive metastatic bone pain. Strontium-89 chloride and samar decline in the potency of an opioid with continued use, ium-153 are available in the United States. Nearly 90% of patients with bone metastasis pres fects in reducing metastatic bone pain, due to their an ent with pain. The duration of pain relief is general comparable in safety prole and eectiveness. Most terminally ill patients with incident temporarily stabilize or improve neurological dysfunc pain found that pain was a major limiting factor to ac tion. The diculty with incident pain is not a lack of in advanced cancer patients for their benets regarding response to systemic opioids, but rather that the doses improved appetite, reduced fatigue, and a sensation of required to control the incident pain produce unaccept well-being, prolonged use should be weighed against able side eects when the patient is at rest. Serious complications of prolonged phine is the primary opioid used in the United States administration of corticosteroids include immunosup for treatment of patients with severe pain in advanced pression, pathological fractures, swelling, and delirium. In the United Kingdom, diamorphine Calcitonin, a hypocalcemic agent, may be use (heroin) is used secondarily because of its greater solu ful as an adjuvant analgesic. Calcitonin inhibits sodium bility, but it has no clinical advantage over morphine. Omar Tawk eect, the role of calcitonin appears to be limited by its prevent loss of bone that occurs from metastatic le short duration of action and poor ecacy due to the sions, reduce the risk of fractures, and decrease pain. Apart from infrequent hypersensitivity reactions eliminate excess calcium through the urine. For mild associated with subcutaneous injections, the main side to-moderate elevations of calcium, patients are usu eect is nausea. For acute Bisphosphonates can delay the onset of skel hypercalcemia, hydration with saline is immediately etal fractures, reduce the need for radiation therapy administered intravenously. The rate of hydration is to treat bone metastasis, reduce hypercalcemia (high based on the severity of the hypercalcemia, the sever blood levels of calcium), and reduce the need for or ity of dehydration, and the ability of the patient to tol thopedic surgery. Furosemide is well tolerated, the strongest activity and is more convenient due to but it is not free of side eects, which may include de reduced administration time. The intravenous method of administration osseous bone pain, such as after radiation damage. Oral tablets are used cyclic antidepressants, such as amitriptyline, are used for maintenance (once or twice a day). Anticonvulsants such as carbamazepine or Prediction of impending fracture and prophylactic clonazepam are particularly useful in neuralgias, such treatment is very important, although prediction itself as in situations with nerve root compression due to remains controversial, with roles advocated both for malignant vertebral body collapse. Increasing uid intake referring the patient to the radiotherapy unit to start ra and the use of diuretics have been standard practice. When this proved insucient, Osseous Metastasis with Incident Pain 153 sustained-release tramadol was added at a dose of 100 Case study (cont. The patient was put on patient-controlled analgesia, us Bisphosphonates (zoledronic acid) at a dose of 4 ing morphine to give her relief from severe pain. She has mg monthly in a drip was prescribed, together with hy been transferred to an orthopedic unit for xation proce dration and advice for the patient to take lots of uids, dures to help relieve her pain and help her to be able to along with furosemide (one tablet daily with a potassium move around. Percutaneous vertebroplasty was done for both L2 and T12, and this procedure was followed by a rapid What can be done by a dedicated relief of back pain.
Purchase 10mg uroxatral amex
They may be spontaneous or provoked by stimulation of the inner thigh or the genitals prostate what is its function purchase 10 mg uroxatral visa. The contractions are usually insufcient, however, to fully evacuate the bladder and the patient must perform an added manoeuvre, either Crede or Valsalva. Detrusor sphincter dyssynergia may require surgical sphincterotomy to remove the resistance to outfow. Bladder training should be started as soon as possible to maintain bladder capacity and compliance. In women, the catheter should be strapped to the thigh so that it lies in a direct line from the bladder outwards. Once the patient begins oral feeding, nutrition must be kept up and the patient weighed and the haemoglobin checked regularly. Patient depression is an important instigating and complicating factor that afects the wish to feed oneself adequately, defeating eforts to establish a proper nutritional status. An H2-receptor antagonist and oral anti-acids should be given to prevent stress ulceration and bleeding during the period of spinal shock. The ileus phase may last several days, only sips of fuid are allowed until peristalsis is well established. Immobility and insufcient fuids may lead to impaction of hard, dry faeces that may proceed all the way to intestinal obstruction. During the stage of spinal shock, an enema may be required several times a week and possibly manual removal of impacted faeces. For the longer term, a high-fuid and adjusted diet with oral stool softeners and bulk forming agents help attain some regularity. Later, laxatives and glycerine suppositories twice weekly can usually replace enemas. Enemas may still be necessary, however, and along with manual disimpaction and removal of faeces, the technique should be taught to the patient and family. Each change of position of the patient in the acute phase should involve breathing exercises and passive movement of the major joints through the full range of fexion and extension. Basic physiotherapy helps prevent atelectasis and hypostatic pneumonia and improves peripheral circulation. It is best not to place pillows under the patient in such a manner as to fex the hips, thus increasing the natural tendency. This aids in mobilization and respiration; it also prepares the patient for eventual vocational training and rehabilitation. Once consolidation of the vertebral fracture and better bladder control have been achieved, the patient may be mobilized to the standing position using posterior plaster-of-Paris splints, followed by gait training with parallel bars, a walking frame, crutches, or simple brace orthoses. The patient should begin using the wheelchair only one or two hours a day, then gradually increase the time in the chair, and be taught to lift and shift the buttocks every 15 minutes. Foam cushions, or better yet an infatable inner tube from a tyre, should be placed on the seat. Some sort of urine control (catheter, condom, disposable incontinence or baby pads) is necessary. Prevention by regular visits of the home-care team and the cooperation of patient and family is best. Even with excellent follow-up complications occur, and the family and team must know when to refer the patient to hospital for further care. The discharge seems to be highly irritant to the intact skin surrounding the ulcer. The surgeon should perform the first wound debridement himself, as necrotic extension in the subcutaneous tissues may underlie intact skin and exploration may be necessary. Infected, deep wounds require regular change of dressings, up to fve times a day, during every other change of patient position. The ulcer should frst be thoroughly washed with copious amounts of normal saline or potable water. Many dressings are available to clean the established ulcer and promote healing, either commercial or based on clinical experience in resource-poor settings. An inexpensive, universally available and efcient dressing to reduce bacterial growth and foul smell is granulated sugar. Another method is to cut out pieces of foam taken from a mattress in the exact shape of the ulcer, wrap in brown sterilization paper and pass through the autoclave. The sterile foam piece is then placed in the ulcer where it absorbs the irritant discharge so that the ulcer bed no longer bathes in it. The foam dressing is changed several times a day depending on the amount of discharge. Local surgical treatment of bedsores is the same as for any other wound: excision of non-viable tissue. Further surgery Large pressure ulcers may require appropriate rotational faps for closure. No fap should be fashioned before the wound area is clean; this may include removing any necrotic bone. The atrophy of the gluteal muscles usually provides a large amount of loose skin that can be mobilized as faps. Superfcial defects can be covered by full-thickness cutaneous faps; deeper areas of defect require musculo-cutaneous faps to obliterate dead space. It should be emphasized that failure of a musculo-cutaneous fap to close a big ulcer often means that there is no second chance since there is not enough skin remaining. Split-skin grafts should not be used as they break down with the slightest pressure afterwards. Musculo-cutaneous faps are highly efective, but surgical experience and good nursing care are essential for good results. Management of incipient pressure sores by the home-care team is described in Annex 36. It is important that the team diagnose the onset of pressure sores early and refer the patient to hospital in good time. In middle to low-income countries, septicaemia and renal failure remain the main causes of death. Audit of the use of sugar dressings for the control of wound odour at Lilongwe Central Hospital, Malawi. Consequently, it is important to prevent urinary tract infection and attain some method of long-term bladder regulation. It is generally brought on by what would have been a noxious stimulus before the injury and is an abnormal autonomic nervous system response. A paradoxical disconnection takes place between peripheral and central mechanisms resulting in a loss of the regulation of blood pressure. The condition may be asymptomatic or result in mild discomfort and headache, or the prolonged bradycardia and severe hypertension may cause retinal haemorrhage, seizures or a cardiovascular accident and death. It is important for hospital staf and the patient to be able to recognize autonomic dysrefexia as it can be a life-threatening condition, especially if it occurs at home and takes patient and family by surprise. The patient should be sat up with the head elevated, any clothing loosened and the cause sought out. The colon should be palpated for a faecal mass, perhaps calling for manual disimpaction.
Purchase generic uroxatral line
However prostate cancer therapy buy uroxatral canada, if patients require therapy for chronic inflammatory General Best Practice Guidelines for Immunization: Altered Immunocompetence 133 conditions, this therapy should not be delayed because of past administration of vaccines (1). Corticosteroid therapy usually is not a contraindication to administering live-virus vaccine when administration is 1) short term. No evidence of an increased risk for more severe reactions to live, attenuated viral vaccines has been reported among persons receiving corticosteroid therapy by aerosol, and such therapy is not a reason to delay vaccination. Other Immunosuppressive Drugs When feasible, clinicians should administer all indicated vaccines before initiation of chemotherapy, before treatment with other immunosuppressive drugs, and before radiation or splenectomy. Persons receiving chemotherapy or radiation for leukemia and other hematopoietic malignancies, or for solid tumors, should be assumed to have altered immunocompetence. Live, attenuated vaccines should not be administered for at least 3 months after such immunosuppressive therapy. Inactivated vaccines administered during chemotherapy should be readministered after immune competence is regained. Children vaccinated before receiving chemotherapy for leukemia, lymphoma, other malignancies, or radiation generally are thought to retain immune memory after treatment, although revaccination with the common childhood vaccines after chemotherapy for acute lymphoblastic leukemia might be indicated (42). Determination of the level of immune memory and the need for revaccination should be made by the treating physician. General Best Practice Guidelines for Immunization: Altered Immunocompetence 134 Certain immunosuppressive medications are administered to prevent solid organ transplant rejection. Live vaccines should be withheld for 2 months following discontinuation of anti-rejection therapies in patients with a solid organ transplant. Zoster vaccine should be withheld one month following discontinuation of anti-rejection therapies (34). Other immunosuppressive medications include human immune mediators like interleukins and colony-stimulating factors, immune modulators, and medicines like tumor necrosis factor-alpha inhibitors and anti-B cell antibodies. Inactivated and live vaccines should be administered 2 or more weeks before initiating such therapies. Live vaccines should be withheld 3 months following such therapies, and both inactivated and live vaccines should be withheld at least 6 months following therapy with anti-B cell antibodies. Anti-B cell antibodies suppress antibody-producing cells for a prolonged duration, hence the longer interval recommended before administering vaccines (17). Zoster vaccine is an exception and should be withheld 1 month following anti-B cell antibodies. An exception is patients with B-cell deficiencies receiving immunoglobulins, who should not receive either live or inactivated vaccines, due to safety (live vaccines) and efficacy (live and inactivated vaccines) concerns. Nonemergency smallpox vaccination is not recommended for children younger than 18 years or the general public. Inactivated influenza vaccine is an exception, but consideration should be given to repeating doses of any inactivated vaccine administered during these therapies. Use of serogroup B meningococcal vaccines in persons aged >/=10 years at increased risk for serogroup B meningococcal disease: recommendations of the Advisory Committee on Immunization Practices, 2015. Use of serogroup B meningococcal vaccines in adolescents and young adults: recommendations of the Advisory Committee on Immunization Practices, 2015. Secondary transmission of varicella vaccine virus in a chronic care facility for children. Chronic progressive poliomyelitis secondary to vaccination of an immunodeficient child. Response of human immunodeficiency virus-infected adults to measles-rubella vaccination. Live virus vaccines in human immunodeficiency virus-infected children: a retrospective survey. Childhood immunization, vaccine preventable diseases and infection with human immunodeficiency virus. Population-based study of measles and measles immunization in human immunodeficiency virus-infected children. Guidelines for preventing infectious complications among hematopoietic cell transplantation recipients: a global perspective. Yellow fever vaccine booster doses: Recommendations of the Advisory Committee on Immunization Practices, 2015. Immunodeficiency in children with acute lymphoblastic leukemia after completion of modern aggressive chemotherapeutic regimens. Special Situations Updates Major revisions to this section of the best practices guidance include the timing of intramuscular administration and the timing of clotting factor deficiency replacement. Concurrent Administration of Antimicrobial Agents and Vaccines With a few exceptions, use of an antimicrobial agent does not interfere with the effectiveness of vaccination. Antibacterial agents have no effect on inactivated, recombinant subunit, or polysaccharide vaccines or toxoids. Ty21a typhoid vaccine should not be administered to persons receiving antimicrobial agents until 72 hours after the last dose of antimicrobial (1). If feasible, to avoid a possible reduction in vaccine effectiveness, antibacterial drugs should not be started or resumed until 1 week after the last dose of Ty21a. Antiviral drugs used for treatment or prophylaxis of influenza virus infections have no effect on the response to inactivated influenza vaccine (2). However, live, attenuated influenza vaccine should not be administered until 48 hours after cessation of therapy with antiviral influenza drugs. These drugs should be discontinued at least 24 hours before administration, if possible. If clinically appropriate, delay use or resumption of antiviral therapy for 14 days after vaccination. If the opportunity to vaccinate might be missed, vaccination should not be delayed only because of these theoretical considerations. For people undergoing serial screening for infection, for instance health care personnel who are tested yearly, differentiation of positive tests due boosting versus new infection is important (9). Active tuberculosis should be considered severe acute illness, and moderate or severe acute illness is a precaution for vaccination. Birth weight and size are not factors in deciding whether to vaccinate a clinically stable preterm infant (11-15), except for hepatitis B vaccination. However, by the chronological age of 1 month, all preterm infants, regardless of initial birth weight, are likely to respond as adequately as larger infants (17-19). The initial vaccine dose should not be counted toward completion of the hepatitis B series, and 3 additional doses of hepatitis B vaccine should be administered, beginning when the infant is aged 1 month. If a child aged at least 6 weeks has been in the hospital since birth, deferral of rotavirus vaccine is recommended until the time of discharge. The rotavirus vaccine series should not be initiated for infants aged 15 weeks, 0 days. Although live viruses in vaccines can replicate in the mother, the majority of live viruses in vaccines have been demonstrated not to be excreted in human milk. Although rubella vaccine virus has been excreted in human milk, the virus usually does not infect the infant. If infection does occur, it is well tolerated because the virus is attenuated (23). Inactivated, recombinant, subunit, polysaccharide, and conjugate vaccines, as well as toxoids, pose no risk for mothers who are breastfeeding or for their infants. Breastfeeding is a contraindication for smallpox vaccination of the mother because of the theoretical risk for contact transmission from mother to infant. In both infants, vaccine virus was recovered from the cerebrospinal fluid of the infant, but the exact mode of transmission was not precisely determined because vaccine virus was not recovered from breast milk (24). However, when nursing mothers cannot avoid or postpone travel to areas endemic for yellow fever in which risk for acquisition is high, these women should be vaccinated.
Purchase uroxatral overnight delivery
Neurological consultation is indicated and further tests for consideration include magnetic resonance angiogram and magnetic resonance venogram prostate icd 10 discount uroxatral 10mg with visa. If the headache is more subacute in onset, chronic meningitis may need to be considered along with a space-occupying intracranial lesion or hydrocephalus. Whether a lumbar puncture is done will be guided by the index of suspicion regarding a meningeal process. It should be treated as an emergency since the possible presence of aneurysmal subarachnoid hemorrhage needs to be assessed as outlined above. The most commonly found lesion is a Chiari malformation, although other posterior fossa lesions are sometimes found. A magnetic resonance imaging needs to be obtained to appropriately investigate for these possibilities. Exertional headache, such as with exercise or during sexual activity, may represent a benign process such as migraine. However, if the headache is severe or thunderclap in onset, inves tigations will be necessary as already outlined above. Of course, this is not universal, and migraine or other primary headache disorders may begin even at an advanced age. Nevertheless, care should be taken before a diagnosis of a primary headache disorder is assigned. Many patients who do have the onset of a new headache disorder after age 50 years will merit brain imaging. In addition, after the age of 50 years, a new headache disorder should evoke suspicion of possible giant cell arteritis. Obviously, symptoms of polymyalgia rheumatica, jaw claudication, scalp tenderness or fever will increase the likelihood of this diagnosis. Findings of frm, nodular temporal arteries and decreased temporal pulses will increase the suspicion, as will an elevated sedimentation rate. Obviously, the differential diagnosis will be long, and the index of suspicion for any given process will largely depend on the clinical setting. For example, meningismus, confusion, altered level of consciousness, memory impairment, papilledema, visual feld defect, cranial nerve abnormalities, pronator drift, extremity weakness, signifcant sensory defcits, refex asymmetry, extensor plantar response, or gait disturbance when accompanying a headache should elicit caution: While neurological signs may be unrelated to a headache, previously undocumented neurological fndings that are presumably new need to be carefully considered. Depending on the index of suspicion, lumbar puncture and blood studies may be indicated. Other etiologies for seizures including space-occupying lesions, infection, stroke and metabolic derangements will need to be considered. Again, magnetic resonance imaging is the imaging procedure of choice unless there is an issue of acute head trauma, in which case a computed tomography head scan should be obtained initially. Findings suggest that the best criteria differentiating migraine from other headache types are the presence of nausea and/or vomiting in combination with two of the following three symptoms: photophobia, phonophobia and osmo phobia (Olesen, 2006 [Reference]). No nausea or vomiting (anorexia may occur) than 4 minutes or two or more symptoms occur in 2. Photophobia and phonophobia are absent, or only one of succession the two is present 3. Previous similar attacks headaches should not have started in close temporal relationship to the disorder. If another disorder is present, the headaches should not have started in close temporal relationship to the disorder. Severe unilateral orbital, supraorbital and/or temporal pain lasting 15 to 180 minutes untreated B. Attack is associated with at least one of the following signs on the side of the pain: 1. Average frequency of greater than 15 attacks per than or equal to 15 days per month for at least three month months* B. Mild to moderate intensity (may inhibit, but aura does not prohibit activities) C. Bilateral location at least three months headache has fulfilled C1 and/or C2 below, that is, has fulfilled criteria for 4. Not aggravated by routine physical activity pain and associated symptoms of migraine without C. No more than one of the following: nausea, (a) unilateral location photophobia or phonophobia (b) pulsating quality D. If another (c) moderate or severe pain intensity disorder is present, the headaches should not have (d) aggravation by or causing avoidance of started in close temporal relationship to the routine physical activity. Treated and relieved by triptan(s) or ergot before the expected development of C1 above D. No medication overuse and not attributed to another causative disorder *Characterization of frequently recurring headache generally requires a headache diary to record information on pain and associated symptoms day by day for at least one month. At least one of the following autonomic features months occurs during exacerbations and ipsilateral to the 2. Migraine-associated symptoms are often misdiagnosed as "sinus headache" by patients and clinicians. While education is of paramount importance in managing any condition, it is especially important in the ongoing management of headache. Patients may have to make lifestyle changes, are often required to make self-management choices in the treatment of individual headaches, and should maintain a diary to clarify the frequency, severity, triggers and treatment responses. Chronic Daily Headache Chronic daily headache refers to the presence of a headache more than 15 days per month for greater than three months. Chronic daily headache is not a diagnosis but a category that may be due to disorders repre senting primary and secondary headaches. Secondary headaches are typically excluded with appropriate neuroimaging and other tests. Chronic daily headache can be divided into those headaches that occur nearly daily that last four hours or less and those that last more than four hours, which is more common. The shorter-duration daily headache contains less-common disorders such as chronic cluster headache and other trigeminal autonomic cephalgias. In the clinic setting, chronic migraine is much more common than chronic tension-type headache. In diary studies, patients who fulfll criteria for a diagnosis of the older defnition of transformed migraine also fulfll criteria for a diagnosis of the revised defnition of chronic migraine, which is presented below (Liebenstein, 2007 [Low Quality Evidence]; Bigal, 2006 [Low Quality Evidence]). Medication-overuse headache When medication overuse is present, this is the most likely cause of chronic headache. Chronic Tension-Type Headache As noted, chronic tension-type headache is much less common than episodic-type headache; it is more likely seen in clinical practice. Hemicrania Continua A less common but not rare (and under recognized) cause for chronic daily headache is hemicrania continua. Hemicrania continua description is a persistent, strictly unilateral headache responsive to indomethacin. This disorder is characterized by its sudden onset, with the patient often able to note the date and time it began. It is typically bilateral and usually resembles migraine or tension-type headache. Other Headache Other headaches include cervicogenic and persistent daily headaches. Additional testing in patients without atypical symptoms or an abnormal neurologic examination is unlikely to be helpful.
Bladder Wrack (Bladderwrack). Uroxatral.
- Thyroid problems including an over-sized thyroid gland (goiter), iodine deficiency, obesity, arthritis, achy joints (rheumatism), hardening of the arteries (arteriosclerosis), digestive problems, "blood cleansing," constipation, and other conditions.
- What is Bladderwrack?
- Are there any interactions with medications?
- Are there safety concerns?
- How does Bladderwrack work?
- Dosing considerations for Bladderwrack.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96710
Generic 10 mg uroxatral amex
Efects of bjsports-2013-092165 of administration of a drugs fail to enhance healing 2018; 129:352-375 prostate quebec purchase generic uroxatral on line. Int J Sports Med [published Online First: basic science to clinical improves the efect of Rev 2015; 84:240-56. Sarimo J, Lempainen the American journal Archives of physical me L, Mattila K, et al. Efcacy of controlled trial of losar injured skeletal muscle Medicine 2017; 27(3):271 Muscle injuries: biology rehabilitation (lengthening) tan as an anti-fbrotic by hyperbaric oxygen 77. Biomechanical considerations that increase the risk of infection: Implantation of a foreign body Known valvular heart disease Indwelling prosthesis 2. Medical considerations that compromise the healing capacity or increase the infection risk: Diabetes Peripheral vascular disease Possibility of gangrene or tetanus Immunocompromised state 3. High-risk wounds or situations: Penetrating wounds Abdominal trauma Compound fractures Wounds with devitalized tissue Lacerations greater than 5 cm or stellate lacerations Contaminated wounds High risk anatomical sites such as hand or foot Biliary and bowel surgery. Immerse towels and drapes for 1 hour in a reliable antiseptic such as aqueous chlorhexidine, wring them out and lay them moist on the skin of the patient. Treat gauze packs and swabs similarly, but rinse them in diluted (1: 1000) chlorhexidine solution before using them in the wound. After use, they should be placed in a special container of disinfectant before being cleaned and sterilized. In most countries, the most widely available disinfectant is sodium hypochlorite solution (commonly known as bleach or chloros), which is a particularly effective antiviral disinfectant solution. However, some disinfectants are themselves inactivated by the presence of organic material and so higher concentrations of disinfectant and longer contact times must be used in certain situations, such as a large spill of infected blood. At the end of the procedure, the outsides of the packs of instruments should not have wet spots, which may indicate that sterilization has not occurred. However, sharp instruments, other delicate equipment and certain catheters and tubes can be sterilized by exposure to formaldehyde, glutaral (glutaraldehyde) or chlorhexidine. Waste disposal in clinical procedures at resource limited health care facility It is essential for the hospital to have protocols for dealing with biological waste and contaminated materials. A three colour coding system with black for non infectious waste, red or yellow for infectious and yellow for sharps is recommended. Whenever feasible plastic material such as syringes or blood bags should not be incinerated. If this is the case, you should do as much as possible to protect the burying site to prevent access and to avoid environmental pollution, especially for underground water sources. This is essential to prevent any unwanted or dangerous reactions between the chemicals, which could endanger laboratory staff. Always follow local guidelines on the disposal of waste chemicals to ensure that chemical contamination of the surrounding land or water supply does not occur. Shock Shock is a pathological, life threatening condition in which the oxygen supply to the tissues of the body fails. Look for unequal pupils or other localizing signs that may show intracranial haematoma developing. However, if a comatose patient has a clear airway and vital signs are normal: Avoid intubation as this will involve drug administration and complicate the subsequent diagnosis Nurse the patient in the recovery position Monitor the airway and await progress and diagnosis (Figure 13. Surgical wound toilet involves: Cleaning the skin with antiseptics Irrigation of wounds with saline Surgical debridement of all dead tissue and foreign matter. Systematically perform wound toilet and surgical debridement, initially to the superficial layers of tissues and subsequently to the deeper layers (Figures 5. Debride the wound meticulously to remove any loose foreign material such as dirt, grass, wood, glass or Figure 5. With a scalpel or dissecting scissors, remove all adherent foreign material along with a thin margin of underlying tissue and then irrigate the wound again. Continue the cycle of surgical debridement and saline irrigation until the wound is completely clean. Pack it lightly with damp saline gauze and cover the packed wound with a dry dressing. Change the packing and dressing daily or more often if the outer dressing becomes damp with blood or other body fluids. If necessary, extend the wound, being careful not to cross skin creases in the palm or digits. Close a clean wound over a drain using interrupted sutures if there is no tension on the skin. Apply a plaster splint to hold the wrist in 20 degrees of extension, with the metacarpophalangeal joints in 90 degrees of flexion and the interphalangeal joints in full extension. To control oedema, elevate the limb for the first week, either by attachment to an overhead frame or by the use of a triangular sling. Before dividing these larger vessels or an end artery, test the effect on the distal circulation by temporary occlusion of the vessel. These sutures should be long enough to assist in tendon or nerve identification at a subsequent procedure. This region may be distorted by the swelling caused by local anaesthetic or blanched by adrenaline, so to assure accuracy, premark the vermillion border with a pen. Use interrupted 4/0 or 3/0 absorbable suture for the inner layers and 4/0 or 5/0 monofilament non absorbable suture in the skin. Lubricate the catheter, and pass it through the nose until the tip reaches the oropharynx. Gently pull the catheter forward until the balloon is held in the posterior choana (Figure 5. Tape the catheter to the forehead or cheek in the same manner as a nasogastric tube.
Discount 10 mg uroxatral
The follow-up Z code categories: Z08 Encounter for follow-up examination after completed treatment for malignant neoplasm Z09 Encounter for follow-up examination after completed treatment for conditions other than malignant neoplasm Z39 Encounter for maternal postpartum care and examination 9) Donor Codes in category Z52 prostate cancer mortality rate discount uroxatral online visa, Donors of organs and tissues, are used for living individuals who are donating blood or other body tissue. Pregnancy, Childbirth, and the Puerperium, for further instruction on the use of these codes. Z codes for pregnancy are for use in those circumstances when none of the problems or complications included in the codes from the Obstetrics chapter exist (a routine prenatal visit or postpartum care). Codes in category Z3A, Weeks of gestation, may be assigned to provide additional information about the pregnancy. Category Z3A codes should not be assigned for pregnancies with abortive outcomes (categories O00-O08), elective termination of pregnancy (code Z33. The date of the admission should be used to determine weeks of gestation for inpatient admissions that encompass more than one gestational week. Z codes/categories for obstetrical and reproductive services: Z30 Encounter for contraceptive management Z31 Encounter for procreative management Z32. The codes are not to be used if the examination is for diagnosis of a suspected condition or for treatment purposes. During a routine exam, should a diagnosis or condition be discovered, it should be coded as an additional code. Pre-existing and chronic conditions and history codes may also be included as additional codes as long as the examination is for administrative purposes and not focused on any particular condition. Pre-operative examination and pre-procedural laboratory examination Z codes are for use only in those situations when a patient is being cleared for a procedure or surgery and no treatment is given. Their use in the outpatient setting should be limited to those instances when there is no further documentation to permit more precise coding. Selection of Principal Diagnosis the circumstances of inpatient admission always govern the selection of principal diagnosis. If no further determination can be made as to which diagnosis should be principal, either diagnosis may be sequenced first. Complications of surgery and other medical care When the admission is for treatment of a complication resulting from surgery or other medical care, the complication code is sequenced as the principal diagnosis. Admissions/Encounters for Rehabilitation When the purpose for the admission/encounter is rehabilitation, sequence first the code for the condition for which the service is being performed. For example, for an admission/encounter for rehabilitation for right-sided dominant hemiplegia following a cerebrovascular infarction, report code I69. If the condition for which the rehabilitation service is no longer present, report the appropriate aftercare code as the first-listed or principal diagnosis, unless the rehabilitation service is being provided following an injury. For example, if a patient with severe degenerative osteoarthritis of the hip, underwent hip replacement and the current encounter/admission is for rehabilitation, report code Z47. If the patient requires rehabilitation post hip replacement for right intertrochanteric femur fracture, report code S72. These data elements and their definitions can be found in the July 31, 1985, Federal Register (Vol. The listing of the diagnoses in the patient record is the responsibility of the attending provider. Previous conditions If the provider has included a diagnosis in the final diagnostic statement, such as the discharge summary or the face sheet, it should ordinarily be coded. Abnormal findings Abnormal findings (laboratory, x-ray, pathologic, and other diagnostic results) are not coded and reported unless the provider indicates their clinical significance. If the findings are outside the normal range and the attending provider has ordered other tests to evaluate the condition or prescribed treatment, it is appropriate to ask the provider whether the abnormal finding should be added. Please note: this differs from the coding practices in the outpatient setting for coding encounters for diagnostic tests that have been interpreted by a provider. The bases for these guidelines are the diagnostic workup, arrangements for further workup or observation, and initial therapeutic approach that correspond most closely with the established diagnosis. Diagnostic Coding and Reporting Guidelines for Outpatient Services these coding guidelines for outpatient diagnoses have been approved for use by hospitals/ providers in coding and reporting hospital-based outpatient services and provider-based office visits. Guidelines in Section I, Conventions, general coding guidelines and chapter-specific guidelines, should also be applied for outpatient services and office visits. Information about the correct sequence to use in finding a code is also described in Section I. The most critical rule involves beginning the search for the correct code assignment through the Alphabetic Index. Never begin searching initially in the Tabular List as this will lead to coding errors. When a patient presents for outpatient surgery and develops complications requiring admission to observation, code the reason for the surgery as the first reported diagnosis (reason for the encounter), followed by codes for the complications as secondary diagnoses. A code is invalid if it has not been coded to the full number of characters required for th that code, including the 7 character, if applicable. In some cases the first-listed diagnosis may be a symptom when a diagnosis has not been established (confirmed) by the physician. Rather, code the condition(s) to the highest degree of certainty for that encounter/visit, such as symptoms, signs, abnormal test results, or other reason for the visit. Code all documented conditions that coexist Code all documented conditions that coexist at the time of the encounter/visit, and require or affect patient care treatment or management. Patients receiving diagnostic services only For patients receiving diagnostic services only during an encounter/visit, sequence first the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the outpatient services provided during the encounter/visit. For encounters for routine laboratory/radiology testing in the absence of any signs, symptoms, or associated diagnosis, assign Z01. For outpatient encounters for diagnostic tests that have been interpreted by a physician, and the final report is available at the time of coding, code any confirmed or definitive diagnosis(es) documented in the interpretation. Patients receiving therapeutic services only For patients receiving therapeutic services only during an encounter/visit, sequence first the diagnosis, condition, problem, or other reason for encounter/visit shown in the medical record to be chiefly responsible for the outpatient services provided during the encounter/visit. The only exception to this rule is that when the primary reason for the admission/encounter is chemotherapy or radiation therapy, the appropriate Z code for the service is listed first, and the diagnosis or problem for which the service is being performed listed second. Patients receiving preoperative evaluations only For patients receiving preoperative evaluations only, sequence first a code from subcategory Z01. Ambulatory surgery For ambulatory surgery, code the diagnosis for which the surgery was performed. An examination with abnormal findings refers to a condition/diagnosis that is newly identified or a change in severity of a chronic condition (such as uncontrolled hypertension, or an acute exacerbation of chronic obstructive pulmonary disease) during a routine physical examination. Medical record documentation from any provider involved in the care and treatment of the patient may be used to support the determination of whether a condition was present on admission or not. General Reporting Requirements All claims involving inpatient admissions to general acute care hospitals or other facilities that are subject to a law or regulation mandating collection of present on admission information. Issues related to inconsistent, missing, conflicting or unclear documentation must still be resolved by the provider.
Uroxatral 10mg otc
Perforation of the diaphragm by a chest tube mounted on a trocar and diagnosis by injection of radio-opaque material prostate cancer 30s buy uroxatral toronto. There are numerous examples in the surgical literature of chest tubes placed with a trocar that have penetrated the lung, mediastinum, heart and great vessels, or an abdominal organ herniated into the chest; or that traversed the diaphragm and punctured the spleen, stomach, or liver. Two sites are classically used for the insertion of a chest tube: midaxillary (basal) and midclavicular (apical) as shown in Figure 31. However, the apical position presents more risks than the basal and should only be resorted to for this condition. If the clinical picture of the patient points to a massive haemothorax with shock, Figure 31. A trained physiotherapist should be present; if not, the surgeon and nursing staf must make certain the patient performs the exercises properly. Functioning of the chest tube the functioning of a chest tube must be checked immediately. The bloody discharge inside the drain and the fuid level in the underwater seal tubing should swing with each breath. If this is not the case, the tube should be inspected to confrm that there has been no dislodgement from the chest wall exposing a side-hole. A chest X-ray soon after inserting the drain is valuable to confrm the following points. Full re-expansion of the lung with complete evacuation of blood and air from the pleural cavity. A second apical chest drain may be required, especially if there is signifcant continuing air leakage. A thoracotomy may be necessary if all the above fail to deal directly with the underlying cause. Daily control X-rays are not absolutely necessary; good clinical examination of the patient is. Care of the chest bottle When the patient is moved or mobilized, care must be taken to make sure the drainage system remains below the level of the chest tube. If it is absolutely necessary to raise it above this level, the tubing should be clamped very briefy. If after clamping the patient becomes dyspnoeic the clamp should immediately be removed. The plastic tubing should not be clasped directly by the clamp, but rather protected by the interposition of a gauze compress. Removal of a chest tube A chest tube should be removed once it has accomplished its task: i. An air leak that slowly decreases and does not require a thoracotomy takes about a week to close. This is a foreign body reaction to the presence of the tube and will continue as long as it is in place. The chest drainage can be removed when the serous discharge falls below 250 ml per day. Warfare within urban areas may allow rapid transport of severely injured patients and therefore lead to a higher rate of thoracotomy. However, the principles of mass casualty triage frequently intervene as well, thus limiting the possibility of performing a thoracotomy. For the surgeon working with limited resources the choice may be between letting a patient die without intervention, or doing the best one can given the prevailing circumstances. Thoracotomy can be an urgent procedure performed as part of resuscitation, an early operation performed after the physiology has been partly restored, or a late surgical intervention usually due to a complication. This in itself strongly argues in favour of thoracotomy being performed only in the oT. Any controversy is largely irrelevant to the general surgeon working with limited resources; under such conditions it is a futile exercise. Better to bring the patient to the operating theatre and, if still alive, with good lighting and instruments and trained personnel, make an attempt at emergency resuscitative thoracotomy there. A sucking chest wound can be brought under control in the emergency department, even if only with a large wet dressing, and the patient taken to theatre immediately. A small wound does not really require a formal thoracotomy, rather debridement with closure of the chest wall and placement of a chest drain. The source of haemorrhage is usually an artery of the chest wall, occasionally a great vessel. A special case is a right-sided exsanguinating thoraco-abdominal wound with dark blood coming from the chest tube. Exploratory laparotomy reveals a retrohepatic venous injury and blood passing through a hole in the diaphragm. A thoracotomy should then be performed and large haemostatic sutures placed to close the hole in the diaphragm from above to allow natural tamponade to occur. A massive air leak due to a major tracheobronchial injury, with collapsed lung on X-ray and continuous bubbling of air throughout the breathing cycle, requires immediate operation as well. Most often encountered is continuing haemorrhage, followed by persistent signifcant air leakage. This bleeding must indeed be coming from a thoracic wound and not from the abdomen through a lesion in the diaphragm. Blood loss through the chest drain, however, is not always a reliable indicator of the total loss; much clotted blood can remain in the pleural cavity if the lung has completely collapsed. Haemorrhage from the intercostal vessels or the low-pressure pulmonary system, even if causing an initial massive haemothorax, often stops. If discharged blood coagulates, the bleeding is ongoing; the fresh blood has not had time to be defbrinogenated by the movement of the lung. If the blood stays fuid, the bleeding has stopped, since the blood draining out has been defbrinogenated. It should be mentioned that the colour of the blood is a poor indicator of ongoing haemorrhage. In a situation where blood for transfusion is in short supply and the surgeon is 31 experienced, some surgeons have argued for an aggressive approach and very early thoracotomy to control bleeding quickly and not let the patient slowly exsanguinate (the Chadian experience described in section 31. Intrapulmonary haematoma Clinical evidence of respiratory distress with an intrapulmonary haematoma larger than 5 cm in diameter on X-ray or increasing in size on serial X-rays is an indication for thoracotomy. Given the additional risk of infection in a large haematoma, a thoracotomy is justifed. In the event of a lung abscess, however, massive antibiotic therapy without thoracotomy is the treatment of choice. In a haemodynamically stable patient, the presence of dyspnoea, surgical emphysema or mediastinal air on X-ray calls for investigation of the oesophagus and trachea. The patient can usually withstand a few hours delay for proper resuscitation and diagnosis.
Order uroxatral 10mg online
Prostate cancer vs hyperplasia: relationships with prostatic and adipose tissue fatty acid composition prostate green light laser surgery purchase cheapest uroxatral. Trabeculation of urinary bladder by ultrasound in patients with benign prostatic hyperplasia. Acinetobacter infections in patients with human immunodeficiency virus infection: microbiological and clinical epidemiology. Cost effectiveness of treatment for benign prostatic hyperplasia: an economic model for comparison of medical, minimally invasive, and surgical therapy. Virtual reality surgical simulation for lower urinary tract endoscopy and procedures. Tretinoin prevents age-related renal changes and stimulates antioxidant defenses in cultured renal mesangial cells. Drug Insight: 5alpha-reductase inhibitors for the treatment of benign prostatic hyperplasia. Prostate volume and serum prostate-specific antigen as predictors of acute urinary retention. Relationship among serum testosterone, sexual function, and response to treatment in men receiving dutasteride for benign prostatic hyperplasia. Eosinophilic crystals as a distinctive morphologic feature of a hyaline droplet nephropathy in a mouse model of acute myelogenous leukaemia. A phase I trial of etanidazole and hyperfractionated radiotherapy in children with diffuse brainstem glioma. Relief by botulinum toxin of voiding dysfunction due to benign prostatic hyperplasia: results of a randomized, placebo-controlled study. Management of bladder, prostatic and pelvic floor disorders with botulinum neurotoxin. Expression of Lewis carbohydrate antigens and chromogranin A in human prostatic cancer. Laparoscopic prostatectomy with vascular control for benign prostatic hyperplasia. Intravesical prostatic protrusion is better than prostate volume in predicting the outcome of trial without catheter in white men presenting with acute urinary retention: a prospective clinical study. Prevalence and correlations of lower urinary tract symptoms, erectile dysfunction and incontinence in men from a multiethnic Asian population: Results of a regional population based survey and comparison with industrialized nations. Bothersome urinary symptoms and disease specific quality of life in patients with benign prostatic obstruction. Multiple doses of saw palmetto (Serenoa repens) did not alter cytochrome P450 2D6 and 3A4 activity in normal volunteers. Use of 5alpha-reductase inhibitors to prevent benign prostatic hyperplasia disease. Tissue effects of saw palmetto and finasteride: use of biopsy cores for in situ quantification of prostatic androgens. Effects of a saw palmetto herbal blend in men with symptomatic benign prostatic hyperplasia. First dose efficacy of alfuzosin once daily in men with symptomatic benign prostatic hyperplasia. The effect of dutasteride on the peripheral and transition zones of the prostate and the value of the transition zone index in predicting treatment response. Doxazosin added to single-drug therapy in hypertensive patients with benign prostatic hypertrophy. Enlarging the scope of managing benign prostatic hyperplasia: addressing sexual function and quality of life. Prostate-specific antigen complexed to alpha(1)-antichymotrypsin in the early detection of prostate cancer. Turbulent urinary flow in the urethra could be a causal factor for benign prostatic hyperplasia. Determination of the percentage of free prostate-specific antigen helps to avoid unnecessary biopsies in men with normal rectal examinations and total prostate-specific antigen of 4-10 ng/ml. Incidental discovery of ano-rectal disease during transrectal ultrasound performed for prostatic disease. Naftopidil monotherapy vs naftopidil and an anticholinergic agent combined therapy for storage symptoms associated with benign prostatic hyperplasia: A prospective randomized controlled study. Renal cell carcinoma: incidental detection during routine ultrasonography in men presenting with lower urinary tract symptoms. The 12-year outcome analysis of an endourethral wallstent for treating benign prostatic hyperplasia. Short-term efficacy and long-term compliance/treatment failure of the alpha1 blocker naftopidil for patients with lower urinary tract symptoms suggestive of benign prostatic hyperplasia. Web-based research of lower urinary tract symptoms that affect quality of life in elderly Japanese men: analysis using a structural equation model. Lower urinary tract symptoms of men seeking medical care-comparison of symptoms found in the clinical setting and in a community study. Natural history of lower urinary tract symptoms in men-result of a longitudinal community-based study in Japan. High plasma norepinephrine levels associated with beta2-adrenoceptor polymorphisms predict future renal damage in nonobese normotensive individuals. Significance of mucin stain in differentiating benign and malignant lesions of prostate. Impact of radical perineal prostatectomy on urinary continence and quality of life: a longitudinal study of Japanese patients. Relationship between the prostatic tissue components and natural history of benign prostatic hyperplasia. Retroperitoneoscopy assisted total nephroureterectomy for upper urinary tract transitional cell carcinoma. Computer simulated additional deep apical biopsy enhances cancer detection in palpably benign prostate gland. Placental growth factor gene expression in human prostate cancer and benign prostate hyperplasia. Diagnostic value of prostate-specific antigen-related parameters in discriminating prostate cancer. Expression of lipoxygenase in human prostate cancer and growth reduction by its inhibitors. Classification of spatial textures in benign and cancerous glandular tissues by stereology and stochastic geometry using artificial neural networks. Nocturia and polyuria in men referred with lower urinary tract symptoms, assessed using a 7-day frequency-volume chart. Combination therapy-permanent interstitial brachytherapy and external beam radiotherapy for patients with localized prostate cancer. Impact of urethral injury management on the treatment and outcome of concurrent pelvic fractures. Five year results from a multicentre randomized controlled trial of endoscopic laser ablation against transurethral resection of the prostate. Transurethral electrovaporization of the prostate: is it any better than conventional transurethral resection of the prostate. Expression of soluble urokinase plasminogen activator receptor may be related to outcome in prostate cancer patients. Ectopic prostatic tissue in the uterine cervix and vagina: report of a series with a detailed immunohistochemical analysis. An economic evaluation of doxazosin, finasteride and combination therapy in the treatment of benign prostatic hyperplasia. Lower urinary tract symptoms suggestive of benign prostatic obstruction-Triumph: health-economical analysis. The appropriateness of treatment of benign prostatic hyperplasia: a comparison of Dutch and multinational criteria. Outcome of primary vesicoureteric reflux detected following fetal renal pelvic dilatation.

Cheap uroxatral
Circulation within the skull is unique in that it is tightly regulated by the blood-brain barrier and is therefore protected against ionic and humoral factors androgen hormone uterine 10 mg uroxatral with visa. The cerebral vasculature undergoes fine adjustments primarily through autoregulatory processes such that under normal healthy conditions on Earth the cerebral blood vessels have an intrinsic ability to keep blood flow constant over a wide range of arterial blood pressure levels via myogenic, metabolic, and tissue pressure mechanisms. Data indicate that upon entry into space, the mean arterial pressure in the head increases from approximately 70 mm Hg to 100 mm Hg. However, a number of studies suggest that cerebral blood flow is lower in response to spaceflight and head-down bed rest (Kawai et al. These differences in the literature highlight the need for additional research in this area. In another study that measured cerebral blood flow, velocities, and beat-to-beat changes in arterial pressure, static autoregulation was not impaired after 16 days in space and, moreover, dynamic regulation (changes occurring during stress) was actually improved (Iwasaki et al. Taken together, these data and recent findings from Jeong and colleagues (Jeong et al. Evidence from several ground-based studies using the rat hind-limb tail suspension model suggests that the reduction in cerebral blood flow is associated with a decrease in autoregulation caused by alterations in cerebral arterial structure and function. Interestingly, the overall functional consequence of increased tone appears to lead to reduced blood flow, and the stimulus does not appear to be an increase in arterial pressure but rather increases in transmural pressure caused by the elevation in the extravascular pressure in the cranium (Wilkerson et al. However, as noted previously, data from similar investigations on cerebral autoregulation in humans during spaceflight do not corroborate the findings in the ground-based analogs. The reason for the profound differences in findings for spaceflight and ground analogs of spaceflight remains unclear; however, it has been speculated that the central volume shift in fluid, and subsequent redistribution of fluid between compartments and tissues is not comparable in these two conditions. Lymphatics Well-regulated lymph function is critical for maintaining normal tissue fluid volume and pressure. The lymphatic system collects excess interstitial fluid and transports this fluid back to the blood through the thoracic duct (Koh et al. Typically, 8 to 12 liters of interstitial fluid are produced daily by transcapillary fluid filtration and transported through the lymphatic vasculature. Cervical lymphatics in the nasal submucosa at the cribriform plate can absorb cerebrospinal fluid (Boulton et al. Because lymph pressures are low (0-20 cm H2O), lymphatic vessels are particularly sensitive to changes in hydrostatic and tissue pressures, which are altered with gravitational changes. It is known that lymphatics from different regions of the body adapt to their regional pressure and flow environments (Gashev et al. For example, 2 weeks of simulated microgravity in rats causes a potent inhibition of pressure/stretch stimulated pumping in all types of lymphatic vessels (Gashev et al. The largest pump flow inhibition was found in cervical lymphatics during simulated microgravity (Gashev et al. These lymphatics use cephalic to thoracic hydrostatic pressure gradient to generate lymph flow. In addition, silicon rubber tracer injected into the subarachnoid space of humans produced extensive infiltration into the lymphatic network adjacent to the extracranial surface of the cribriform plate and optic nerve (Johnston 2003; Koh et al. In fact, ligation of the cervical lymphatics result in edema of the brain and protein accumulation (Casley-Smith et al. However, it is unclear how impaired lymphatic function may contribute to vision impairment. Glymphatics the central nervous system does not contain traditional lymphatic vasculature. From this perivenous space, the interstitial fluid can then empty into the cervical lymphatic system (Johnston et al. Data suggest that lipids and lipoproteins greater than 1 kDa are localized to the perivascular space of the brain, and astrocytes release carrier proteins, thus the glymphatic pathway provides a route for lipid distribution. Rodent data suggest that the glymphatic pathways become enhanced during sleep, evidenced by the change in volume fraction of interstitial space of 14% during wake and 23% during sleep (Xie et al. Posture may play an additional role in the ability for the glymphatic system to clear waste during sleep. It remains to be determined if and how a spaceflight-induced glymphatic dysfunction might play a role in the spaceflight-induced vision impairment. Denniston and Keane proposed that the paravascular system of the retina may be critical in retinal disease. Ventricular volume changes from pre to post-bed rest were seen in some subjects, but due to the large variability between individuals a change in ventricular volume for the group as a whole was not statistically significance. However, these authors suggested an association between brain rotation and percent change in ventricle volume. Moreover, there was a significant increase in both gray and white matter density at the brain vertex. Cine clips of matched pre and post-flight images of 18 astronauts revealed narrowing of the central sulcus, enlargement of the ventricular system (lateral, third, and fourth ventricles), and a more frequent upward shift of the brain in long duration (n=12) compared to short-duration (n=6) fliers. Indeed, further research is needed to explore this hypothesis and determine if these structural changes that appear in long-duration crewmembers represent pathological findings or are subclinical findings from exposure to prolonged weightlessness and resolve with time after return to a 1g environment. It remains unknown if the structural changes and movement of the brain within the skull following bed rest or spaceflight result in alterations to venous outflow from the brain. Some potential compressive zones have also been proposed as possibly relevant in contributing to the venous congestion in microgravity (Wiener 2012). This suggests these female subjects experienced a greater translaminar pressure gradient in the posterior direction. Whether this difference between sexes occurs in astronauts during spaceflight and helps protect against the stimuli causing globe flattening is unknown and this hypothesis requires further investigation. To date, 24 individual United States and partner agency astronauts have demonstrated one or more of the following signs: optic disc edema, globe flattening, choroidal folds, cotton wool spots, and/or change in refractive error. This hypothesis should be given greater investigative interest than it has previously received. As more optical coherence tomography images (which provide the most detailed and quantitative assessment of the posterior globe) are collected, we will develop a better understanding of the spatial and temporal time course of structural ocular changes. Targeting the venous system that drains the head, the lymphatic system, and possible changes in cerebral spinal fluid all represent areas of research for possible countermeasure development or areas that may provide mechanistic insight that have not been fully investigated thus far. Studies are currently underway to investigate the use of devices that redistribute fluids distally, including Braslet thigh cuffs, a modified version of the Kaatsu system, an impedance threshold device, artificial gravity, and a lower body negative pressure device. B5 Gabrion J, Herbute S, Oliver J, et al (1995) Choroidal responses in microgravity.

