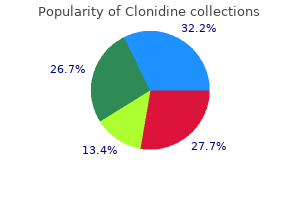
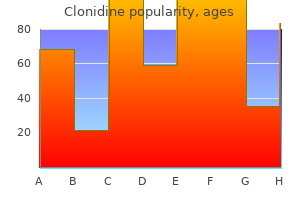
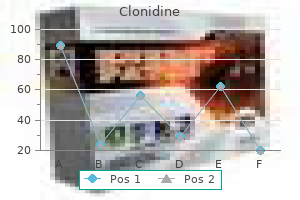
Clonidine
Purchase clonidine 0.1mg free shipping
Infammatory syndromes (pericarditis and rheumatologic syndromes) also can develop; erythema nodosum can occur in adolescents and adults arrhythmia emedicine discount clonidine 0.1mg without prescription. H capsulatum var duboisii is the cause of African histoplasmosis and is found only in central and western Africa. Infection is acquired through inhalation of conidia from soil, often contaminated with bat guano or bird droppings. The inoculum size, strain virulence, and immune status of the host affect severity of illness. Infections occur sporadically, in outbreaks when weather condi tions (dry and windy) predispose to spread of spores or as point-source epidemics after exposure to activities that disturb contaminated soil. Prior infection confers partial immunity; reinfection can occur but requires a larger inoculum. H capsulatum organ isms from bone marrow, blood, sputum, and tissue specimens grow on standard mycologic media in 1 to 6 weeks. Demonstration of typical intracellular yeast forms by examination with Gomori methenamine silver or other stains of tissue, blood, bone marrow, or bronchoalveolar lavage specimens strongly supports the diagnosis of histoplasmosis when clinical, epide miologic, and other laboratory studies are compatible. Detection of H capsulatum antigen in serum, urine, a bronchoalveolar lavage speci men, or cerebrospinal fuid using a quantitative enzyme immunoassay is possible using a rapid, commercially available diagnostic test. Antigen detection in blood and urine specimens is most sensitive for severe, acute pulmonary infections and for progressive disseminated infections. Results often transiently are positive early in the course of acute, self-limited pulmonary infections. If the result initially is positive, the antigen test also is useful for monitoring treatment response and, after treatment, identifying relapse. Cross-reactions occur in patients with blastomy cosis, coccidioidomycosis, paracoccidioidomycosis, and penicilliosis; clinical and epide miologic circumstances aid in differentiating these infections. Serologic testing also is available and is most useful in patients with subacute or chronic pulmonary disease. A fourfold increase in either yeast-phase or mycelial-phase titers or a single titer of 1:32 in either test is presumptive evidence of active or recent infection. Cross-reacting antibodies can result from Blastomyces dermatitidis and Coccidioides species infections. The immunodiffusion test is more specifc than the complement fxa tion test, but the complement fxation test is more sensitive. Itraconazole 1 is preferred over other azoles by most experts; when used in adults, itraconazole is more effective, has fewer adverse effects, and is less likely to induce resistance than fuconazole. Although safety and effcacy of itraconazole for use in children have not been established, anecdotal experience has found it to be well tolerated and effective. Serum concentrations of itraconazole should be determined to ensure that effective, nontoxic levels are attained. Immunocompetent children with uncomplicated acute pulmonary histoplasmosis rarely require antifungal therapy, because infection usually is self-limited. If the patient is symptomatic for more than 4 weeks, itraconazole should be given for 6 to 12 weeks, although the effectiveness of this treatment is not well documented. For severe acute pulmonary infections, treatment with amphotericin B is recommended for 1 to 2 weeks. After clinical improvement occurs, itraconazole is recommended for an additional 12 weeks. Methylprednisolone during the frst 1 to 2 weeks of therapy can be used if respira tory complications develop. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Severe cases initially should be treated with amphotericin B followed by itraconazole for the same duration. Mediastinal and infammatory manifestations of infection generally do not need to be treated with antifungal agents. However, mediastinal adenitis that causes obstruction of a bronchus, the esophagus, or another mediastinal structure may improve with a brief course of corticosteroids. In these instances, itraconazole should be used concurrently and continued for 6 to 12 weeks. Dense fbrosis of mediastinal structures without an associated granulomatous infammatory component does not respond to antifungal therapy, and surgical intervention may be necessary. Pericarditis and rheumatologic syndromes may respond to treatment with nonsteroidal anti-infammatory agents (indomethacin). For treatment of progressive disseminated histoplasmosis in a nonimmunocompro mised infant or child, amphotericin B is the drug of choice and is given for 4 to 6 weeks. An alternative regimen uses induction with amphotericin B therapy for 2 to 4 weeks and, when there has been substantial clinical improvement and a decline in the serum concen tration of histoplasmosis antigen, oral itraconazole is administered for 12 weeks. Longer periods of therapy can be required for patients with severe disease, primary immunode fciency syndromes, acquired immunodefciency that cannot be reversed, or patients who experience relapse despite appropriate therapy. Stable, low concentra tions of urine antigen that are not accompanied by signs of active infection may not nec essarily require prolongation or resumption of treatment. Exposure to soil and dust from areas with signifcant accumulations of bird and bat droppings should be avoided, especially by immunocompromised people. If exposure is unavoidable, it should be minimized through use of appropriate respiratory protec tion (eg, N95 respirator), gloves, and disposable clothing. Old structures likely to have been contaminated with bird or bat droppings should be moistened thoroughly before demolition. Guidelines for preventing histoplasmosis have been designed for health and safety professionals, environmental consultants, and people supervising workers involved in activities in which contaminated materials are disturbed. Chronic hookworm infection in children may lead to physical growth delay, defcits in cognition, and developmental delay. Pneumonitis associated with migrating larvae is uncommon and usually mild, except in heavy infections. Colicky abdominal pain, nausea, and/or diarrhea and marked eosinophilia can develop 4 to 6 weeks after exposure. Blood loss secondary to hookworm infection develops 10 to 12 weeks after initial infection and symptoms related to serious iron-defciency anemia can develop in long-standing moder ate or heavy hookworm infections. After oral ingestion of infectious Ancylostoma duodenale larvae, disease can manifest with pharyngeal itching, hoarseness, nausea, and vomiting shortly after ingestion. Hookworms are prominent in rural, tropical, and subtropical areas where soil contamination with human feces is common. Although the prevalence of both hookworm species is equal in many areas, A duodenale is the predominant species in the Mediterranean region, northern Asia, and selected foci of South America. N americanus is predominant in the Western hemisphere, sub-Saharan Africa, Southeast Asia, and a number of Pacifc islands. These larvae develop into infective flariform larvae in soil within 5 to 7 days and can persist for weeks to months. A duodenale transmission can occur by oral ingestion and possibly through human milk. Approximately 5 to 8 weeks are required after infection for eggs to appear in feces. A direct stool smear with saline solution or potas sium iodide saturated with iodine is adequate for diagnosis of heavy hookworm infection; light infections require concentration techniques. Quantifcation techniques (eg, Kato Katz, Beaver direct smear, or Stoll egg-counting techniques) to determine the clinical signifcance of infection and the response to treatment may be available from state or reference laboratories. Although data suggest that these drugs are safe in children younger than 2 years of age, the risks and benefts of therapy should be con sidered before administration. In 1-year-old children, the World Health Organization recommends reducing the albendazole dose to half of that given to older children and adults. Reexamination of stool specimens 2 weeks after therapy to deter mine whether worms have been eliminated is helpful for assessing response to therapy. Nutritional supplementation, including iron, is important when severe anemia is present. Treatment of all known infected people and screening of high-risk groups (ie, children and agricultural workers) in areas with endemic infection can help decrease environmental contamination. Wearing shoes may not be fully protective, because cutaneous exposure to hookworm larvae over the entire body surface of children could result in infection. Despite relatively rapid reinfection, periodic deworming treatments targeting preschool-aged and school-aged children have been advocated to prevent morbidity associated with heavy intestinal helminth infections.
Diseases
- Multiple congenital contractures
- Epidermolysis bullosa dystrophica, dominant type
- Egg shaped pupils
- Mycobacterium avium complex infection
- Chromosome 3 duplication syndrome
- Macrocephaly short stature paraplegia
- McDowall syndrome
- Congenital muscular dystrophy syringomyelia
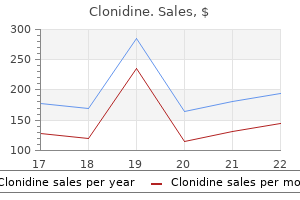
Purchase clonidine 0.1mg with mastercard
Hairs and scale obtained by gentle scraping of a moistened area of the scalp with a blunt scalpel ulterior motive synonym buy clonidine 0.1mg overnight delivery, toothbrush, brush, tweezers, or a moistened cotton swab are used for potassium hydroxide wet mount examination and culture. In cases of T tonsurans infection, microscopic examination of a potassium hydroxide wet mount preparation will disclose numerous arthroconidia within the hair shaft. Use of dermatophyte test medium also is a reliable, simple, and inexpensive method of diagnosing tinea capitis. Skin scrapings, brushings, or hairs from lesions are inoculated directly onto culture medium and incubated at room tempera ture. When necessary, diagnosis also may be confrmed by culture on Sabouraud dextrose agar by direct plating technique or by samples collected on cotton-tipped applicators and transported to reference laboratories. Periodic acid-Schiff staining of histopathologic specimens and polymerase chain reac tion evaluation are possible in academic centers but are expensive and rarely required for confrmation. Examination of hair of patients with Microsporum infection under Wood light results in brilliant green fuorescence. However, because T tonsurans does not fuoresce under Wood light, this diagnostic test is not helpful for most patients with tinea capitis. Microsize griseofulvin, 20 mg/kg per day (maximum, 1 g), or ultramicrosize griseofulvin, 10 to 15 mg/kg per day (maximum, 750 mg), is administered orally, once daily. Optimally, griseofulvin is given after a meal containing fat (eg, peanut butter or ice cream). Treatment typically is necessary for 4 to 6 weeks and should be continued for 2 weeks beyond clinical resolution. Children who have no history or clinical evidence of liver dis ease are not required to have serum hepatic enzyme values tested either before or during a standard course of therapy lasting up to 8 weeks. Prolonged therapy may be associated with a greater risk of hepatotoxicity, and enzyme testing every 8 weeks during treatment should be considered. Terbinafne dosage is based on body weight, and a pediatric granule formulation is available in 125-mg and 187. Baseline serum transaminase (alanine transaminase and aspartate transaminase) testing is advised. Terbinafne tablets, used off-label for tinea capitis, often are dosed on a weight-based sliding scale (67. In addition, off label treatment with oral itraconazole or fuconazole may be effective for tinea capitis; itraconazole is not approved for use in children. Microsporum infections are more likely to respond to griseofulvin, and Trichophyton infections are more likely to respond to terbin afne. Kerion can be treated with griseofulvin; terbinafne may be used if a Trichophyton species is the pathogen. Corticosteroid therapy consisting of prednisone or predniso lone administered orally in dosages of 1. Treatment with a corticosteroid should be continued for approximately 2 weeks, with tapering doses toward the end of therapy. Antibacterial agents generally are not needed, except if there is suspected sec ondary infection. Families should be queried regarding other symptomatic members, and examination performed on such individu als. People with tinea capitis should not return to wrestling for 14 days after commencing systemic therapy. Children receiving treatment for tinea capitis may attend school once they start ther apy with griseofulvin, terbinafne, or other effective systemic agent, with or without the addition of selenium sulfde shampoo. The lesion often is ring-shaped or circular (hence, the term ringworm), slightly erythematous, and well demarcated with a scaly, vesicular, or pustular border. Small confuent plaques or papules as well as multiple lesions can occur, particularly in wrestlers (tinea gladiatorum). Lesions can be mistaken for psoriasis, pityriasis rosea, or atopic, seborrheic, or contact dermatitis. A frequent source of confusion is an alteration in the appearance of lesions as a result of application of a topical corticosteroid preparation, termed tinea incognito. Such patients may also develop Majocchi granuloma, a follicular fungal infection associated with a granuloma tous dermal reaction. A pruritic, fne, papulovesicular eruption (dermatophytic or id reaction) involving the trunk, hands, or face, caused by a hypersensitivity response to infecting fungus, may accompany skin lesions. Tinea corporis can occur in association with tinea capitis, and examination of the scalp should be performed, particularly in affected wrestlers and people who have lesions on the neck and face. The incubation period is thought to be 1 to 3 weeks but can be shorter, as docu mented infections have occurred at 6 days of life in infants with unaffected mothers. Use of dermatophyte test medium also is a reliable, simple, and inexpensive method of diagnosis. Skin scrap ings from lesions are inoculated directly onto culture medium and incubated at room temperature. After 1 to 2 weeks, a phenol red indicator in the agar will turn from yellow to red in the area surrounding a dermatophyte colony. When necessary, the diagnosis also can be confrmed by culture on Sabouraud dextrose agar. Histopathologic diagnosis using periodic acid-Schiff staining and polymerase chain reaction diagnostic tools are available but are expensive and generally unnecessary. Although clinical resolution may be evident within 2 weeks of therapy, continuing therapy for another 2 to 4 weeks generally is recommended. If signifcant clin ical improvement is not seen after 4 to 6 weeks of treatment, an alternate diagnosis should be considered. Topical preparations of antifungal medication mixed with high-potency corticosteroids should not be used, because these often are less effective and can lead to a more deep-seated follicular infection (Majocchi granuloma); in addition, local and sys temic adverse events from the corticosteroids can occur. If lesions are extensive or unresponsive to topical therapy, griseofulvin is administered orally for 4 weeks (see Tinea Capitis, p 712). People with corporis tinea should not return to wrestling for 72 hours after commence ment of topical therapy. Periodic inspections of contacts for early lesions and prompt therapy are recommended. Wrestling mats and equipment should be cleaned frequently, and actively infected wrestlers must be excluded from competitions. The eruption usually is bilaterally symmetric and sharply marginated, often with polycyclic borders. Involved skin is erythematous and scaly and varies from red to brown; occasionally, the eruption is accompanied by central clear ing and a vesiculopapular border. In chronic infections, the margin may be subtle, and lichenifcation may be present. These lesions should be differentiated from candidiasis, intertrigo, seborrheic dermatitis, psoriasis, atopic dermatitis, irritant or allergic contact dermatitis (generally caused by therapeutic agents applied to the area), and erythrasma. The latter is a superfcial bacte rial infection of the skin caused by Corynebacterium minutissimum. This infection commonly occurs in association with tinea pedis, and all infected patients should be evaluated for this possibility, with careful evalua tion of the interdigital web spaces. Onychomycosis also is a possible association, particu larly in adolescents and adults. Use of dermatophyte test medium also is a reliable, simple, and inexpensive method of diagnosing tinea cruris. Skin scrapings from lesions are inoculated directly onto culture medium and incubated at room temperature. When necessary, the diag nosis also can be confrmed by culture on Sabouraud dextrose agar. Polymerase chain reaction assay is a more expensive diagnostic tool that generally is not required. A charac teristic coral-red fuorescence under Wood light can identify the presence of erythrasma (an eruption of reddish brown patches attributable to the presence of Corynebacterium minutissimum) and, thus, exclude tinea cruris. Once-daily therapy with topical econazole, ketoconazole, naftifne, oxiconazole, butenafne (12 years of age and older), or sulconazole preparation also is effective (see Topical Drugs for Superfcial Fungal Infections, p 836). Tinea pedis, if present, should be treated concur rently (see Tinea Pedis, p 717). Topical preparations of antifungal medication mixed with high-potency corticoste roids should be avoided because of the potential for prolonged infections and local and systemic adverse corticosteroid-induced events. Loose-ftting, washed cotton underclothes to decrease chafng as well as the use of an absorbent powder can be helpful adjuvants to therapy.
Cheap clonidine 0.1mg overnight delivery
Drug susceptibility testing of the organism recovered from the mother or household contact heart attack jack ps baby buy clonidine mastercard, infant, or both should be performed. Management of the newborn infant is based on categorization of the maternal (or household contact) infection. Although protection of the infant from exposure and infection is of paramount importance, contact between infant and mother should be allowed when possible. Cases of suspected or proven tuberculosis disease in mothers (or household contacts) should be reported immediately to the local health department, and investigation of all household members should start within 7 days. The mother (or household con tact) and the infant should be separated until the mother (or household contact) has been evaluated and, if tuberculosis disease is suspected, until the mother (or household contact) and infant are receiving appropriate antituberculosis therapy, the mother wears a mask, and the mother understands and is willing to adhere to infection-control measures. Women with tuberculosis disease who have been treated appro priately for 2 or more weeks and who are not considered contagious can breastfeed. If tuberculosis disease is excluded, isoniazid should be continued for a total of 9 months. If the chest radiograph of the mother (or household contact) appears abnormal but is not suggestive of tuberculosis disease and the history, physical examination, and sputum smear indicate no evidence of tuber culosis disease, the infant can be assumed to be at low risk of tuberculosis infection and need not be separated from the mother (or household contact). Infection-control measures for hospital personnel exposed to contagious patients should include the use of personally ftted and sealed particulate respirators for all patient contacts (see Infection Control for Hospitalized Children, p 160). The contagious patient should be placed in an airborne infection isolation room in the hospital. The major concern in infection control relates to adult household members and con tacts who can be the source of infection. Household members and contacts should be managed with tuberculosis precautions when visiting until they are demonstrated not to have contagious tuberculosis. Nonadherent household contacts should be excluded from hospital visitation until evaluation is complete and tuberculosis disease is excluded or treatment has ren dered source cases noncontagious. Children who come from countries where M bovis is prevalent in cattle or whose parents come from those countries are more likely to be infected. Most infections in humans are transmitted from cattle by unpasteur ized milk and its products, such as fresh cheese, although human-to-human transmission by the airborne route has been documented. In children, M bovis more commonly causes cervical lymphadenitis, intestinal tuberculosis disease, and meningitis. In adults, latent M bovis infection can progress to advanced pulmonary disease, with a risk of transmission to others. This approach can be unreliable, and species confrmation at a reference labora tory should be requested when M bovis is suspected. Molecular genotyping through the state health department may assist in identifying M bovis. Controlled clinical trials for treatment of M bovis disease have not been conducted, and treatment recommendations for M bovis disease in adults and children are based on results from treatment trials for M tuberculosis disease. Initial therapy should include 3 or 4 drugs besides pyrazinamide that would be used to treat disease from M tuberculosis infection. For isoniazid and rifampin-susceptible strains, a total treatment course of at least 9 to 12 months is recommended. Parents should be counseled about the many infectious diseases transmitted by unpas teurized milk and its products, and parents who might import traditional dairy products from countries where M bovis infection is prevalent in cattle should be advised against giving those products to their children. When people are exposed to an adult who has pulmonary disease caused by M bovis infection, they should be evaluated by the same methods as other contacts to contagious tuberculosis. A plan to control and prevent extensively drug-resistant tuberculosis has been published. Eliminating ingestion 2 of unpasteurized dairy products will prevent most M bovis infection. Because children with tuberculosis usually are not contagious unless they have an adult type multibacillary form of pulmonary or laryngeal disease, their contacts are not likely to be infected unless they also have been in contact with an adult source case. After the presumptive adult source of the childs tuberculosis is identifed, other contacts of that adult should be evaluated. Plan to combat extensively drug-resistant tuberculosis: recom mendations of the Federal Tuberculosis Task Force. Guidelines for the investigation of contacts of persons with infectious tuberculosis. Children with tuberculosis disease can attend school or child care if they are receiving therapy (see Children in Out-of-Home Child Care, p 133). They can return to regular activities as soon as effective therapy has been instituted, adherence to therapy has been documented, and clinical symptoms have diminished. The protective effcacy against pulmonary tuberculosis differed signifcantly among the studies, precluding a specifc conclusion. Disseminated fatal infection occurs rarely (approximately 2 per 1 million people), primarily in people who are immunocompromised severely. Reporting of suspected and confrmed cases of tuberculosis disease is mandated by law in all states. Physicians should assist local health department personnel in the search for a source case and others infected by the source case. Members of the household, such as relatives, babysitters, au pairs, boarders, domestic workers, and frequent visitors or other adults, such as child care providers and teachers with whom the child has frequent contact, potentially are source cases. Less common syndromes include soft tissue infection, osteomyelitis, otitis media, central line catheter-associated bloodstream infections, and pulmonary infection, espe cially in adolescents with cystic fbrosis. Symptoms can include worsening fever, swollen lymph nodes, local pain, and laboratory abnormalities. Several new species that can be detected by nucleic acid amplifcation testing but cannot be grown by routine culture methods have been identifed in lymph nodes of children with cervical adenitis. Rapidly growing mycobacteria have been implicated in wound, soft tissue, bone, pulmonary, central venous catheter, and middle-ear infections. Other mycobacterial species that usually are not pathogenic have caused infections in immunocompromised hosts or have been associated with the presence of a foreign body. Tap water is the major reservoir for Mycobacterium kansasii, Mycobacterium lentefavum, Mycobacterium xenopi, Mycobacterium simiae, and health care associated infections attributable to the rapidly growing mycobacteria M abscessus and M fortuitum. For M marinum, water in a fsh tank or aquarium or an injury in a salt water environment are the major sources of infection. Pulmonary disease and rare cases of mediastinal adenitis and endobronchial disease do occur. Most infections remain localized at the portal of entry or in regional lymph nodes. Outbreaks of otitis media caused by M abscessus have been associated with polyethylene ear tubes and use of contaminated equipment or water. Buruli ulcer disease is a skin and bone infection caused by Mycobacterium ulcerans, an emerg ing disease causing signifcant morbidity and disability in tropical areas such as Africa, Asia, South America, Australia, and the western Pacifc. Consultation with the laboratory should occur to ensure that culture specimens are handled correctly. For example, isolation of Mycobacterium haemophilum requires that the culture be maintained at 25C. Because these organisms commonly are found in the envi ronment, contamination of cultures or transient colonization can occur. Caution must be exercised in interpretation of cultures obtained from nonsterile sites, such as gastric wash ing specimens, endoscopy material, a single expectorated sputum sample, or urine speci mens and if the species cultured usually is nonpathogenic (eg, Mycobacterium terrae complex or Mycobacterium gordonae). An acid-fast bacilli smear-positive sample or repeated isolation of a single species on culture media is more likely to indicate disease than are culture contamination or transient colonization. Recovery of 1 American Thoracic Society and Infectious Disease Society of America. The interferon-gamma release assays use 2 or 3 antigens to detect infection with M tuberculosis. Although these antigens are not found on M avium-intracellulare, cross reactions can occur with infection caused by M kansasii, M mari num, and Mycobacterium szulgai (See Tuberculosis, p 736). Antimicrobial therapy has been shown in a randomized, controlled trial to provide no additional beneft. Therapy with clarithromycin or azithromycin combined with ethambutol or rifampin or rifabutin may be benefcial for children in whom surgical excision is incomplete or for children with recurrent disease (see Table 3. Isolates of rapidly growing mycobacteria (M fortuitum, M abscessus, and M chelonae) should be tested in vitro against drugs to which they commonly are susceptible and that have been used with some therapeutic success (eg, amikacin, imipenem, sulfamethoxazole or trimethoprim-sulfamethoxazole, cefoxitin, ciprofoxacin, clarithromycin, linezolid, and doxycycline). Clarithromycin and at least one other agent is the treatment of choice for 1 cutaneous (disseminated) infections attributable to M chelonae or M abscessus. Indwelling foreign bodies should be removed, and surgical debridement for serious localized disease is optimal. The decision to embark on therapy should take into consideration susceptibility testing results and involve consultation with an expert in cystic fbrosis care.
Buy 0.1 mg clonidine with amex
Because of the associated anaesthesia and abdominal oestradiol levels may precipitate a prothrombotic state hypertension headache buy clonidine with american express. Congenital heart disease and pulmonary hypertension Table 9 General recommendations In many women with congenital heart disease, pregnancy is well tolerated. The risk of pregnancy depends on the underlying Recommendations Classa Levelb heart disease as well as on additional factors such as ventricular Pre-pregnancy risk assessment and counselling and valvular function, functional class, and cyanosis. The miscar is indicated in all women with known or riage rate is higher in more complex disease (Figure 1). High risk patients should be treated in I C Offspring complications, including offspring mortality (4%), are specialized centres by a multidisciplinary team. Diagnosis Echocardiography should be performed in any pregnant patient with unexplained or new I C Usually, congenital heart diseases will be known and diagnosed cardiovascular signs or symptoms. Pre-pregnancy assessment including medical Before cardiac surgery a full course of history, echocardiography, and exercise testing is indicated in all corticosteroids should be administered to the I C patients, with other diagnostic tests indicated on an individual mother whenever possible. Functional status before pregnancy and history of For the prevention of infective endocarditis in pregnancy the same measures as in non I C previous cardiac events are of particular prognostic value (see pregnant patients should be used. Diagnostic procedures that can be used during pregnancy are When gestational age is at least 28 weeks, 21 outlined in Section 2. This occurs even in patients with little or no dis hypoxia, and acidosis which may precipitate refractory heart ability before or during pregnancy. Supplemental oxygen therapy should be given if there is are: late hospitalization, severity of pulmonary hypertension, and 87 hypoxaemia. The risk probably increases with more elev occasionally used antenatally and peripartum to improve haemody ated pulmonary pressures. In patients where the indication for anticoagulation basis of all available diagnostic modalities in a specialized centre. In portal hypertension, anticoagulation is not recommended in view of the risks of anaesthesia this should be performed in a patients with increased risk of bleeding. It oxygen saturation is,85%, a substantial maternal and fetal mor should be recognized that potentially signicant drug interactions tality risk is expected and pregnancy is contraindicated. Planned the degree of maternal hypoxaemia is the most important predic caesarean delivery and vaginal delivery are favoured over emer tor of fetal outcome. If, however, maternal oxygen saturation is,85%, the chance of a live birth is 91 3. Maternal risk Eisenmenger patients need special consideration because of the Management association of pulmonary hypertension with cyanosis due to the Follow-up. Systemic vasodilatation increases the plemental oxygen (monitoring oxygen saturation) are rec right-to-left shunt and decreases pulmonary ow, leading to ommended. Because of the increased risk of paradoxical increased cyanosis and eventually to a low output state. The litera embolism, prevention of venous stasis (use of compression stock ings and avoiding the supine position) is important. Thrombo-embolism is a major risk for Obstetric and offspring risk cyanotic patients, therefore patients should be considered for pro Cyanosis poses a signicant risk to the fetus, with a live birth unli phylaxis after haematology review and investigations for blood kely (,12%) if oxygen saturation is,85%. When pregnancy occurs, the risks should be discussed cated and managed in the same way as in patients with Eisenmen and a termination of pregnancy offered; however, termination ger syndrome. If the patient wishes to continue with preg nancy, care should be based in a specialist unit. Thrombo-embolism is a major risk for cyanotic patients, fetal condition deteriorates, an early caesarean delivery should be therefore patients should be considered for prophylaxis after hae planned. In view of the risks of anaesthesia this should be per matology review and investigations for blood haemostasis. Antic formed in a tertiary centre experienced in the management of oagulation must be used with caution, as patients with these patients. In others, timely hospital admission, planned elec Eisenmenger syndrome are also prone to haemoptysis and throm tive delivery, and incremental regional anaesthesia may improve maternal outcome. The risks and benets of anticoagulation must there fore be carefully considered on an individual patient basis. It may be valvular, supravalvular, or caused by oxygen saturation measurement and full blood count are indicated. The manage ment of supravalvular and subvalvular stenosis is only described in Delivery. If the maternal or fetal condition deteriorates, an early case reports during pregnancy and is probably similar to the man caesarean delivery should be planned. In view of the risks of anaes thesia this should be performed in a tertiary centre experienced in agement of patients with valvular stenosis, although balloon valvu 92 the management of these patients. Although patients need pregnancy evaluation of the presence of a (residual) defect, to be informed about the (often small) additional risk, pregnancy cardiac dimensions, and an estimation of pulmonary pressures is should not be discouraged. The Obstetric and offspring risk follow-up plan should be individualized taking into account the Pre-eclampsia may occur more often than in the normal complexity of the heart disease and clinical status of the patient. The risk of heart failure is low and only exists in women with severe regur gitation or impaired ventricular function. Offspring mortality has been reported in 6%, primarily due to the occurrence of complex con 99 genital heart disease. For a secun Management dum defect, catheter device closure can be performed during preg Follow-up. Follow-up during pregnancy is advisable at least once nancy, but is only indicated when the condition of the mother is each trimester. Clinical and echocardiographic follow-up is indi deteriorating (with transoesophageal or intracardiac echocardio cated monthly or bimonthly in patients with moderate or severe graphic guidance). For rec Because of the increased risk of paradoxical embolism, in ommended preventive measures for thrombo-embolism, see women with a residual shunt, prevention of venous stasis (use of Section 3. Pregnancy is often well tolerated in women after repair of coarcta Spontaneous vaginal delivery is in most cases appropriate. Other risk factors for this complication include aortic dilatation and bicuspid aortic valve, and they 3. The Obstetric and offspring risk rate of progression of stenosis in these young patients is lower 107 An excess of hypertensive disorders and miscarriages has been than in older patients. Hypertension should be treated, undergo imaging of the ascending aorta before pregnancy, and although aggressive treatment in women with residual coarctation surgery should be considered when the aortic diameter is must be avoided to prevent placental hypoperfusion. The use of covered stents may lower the risk In unrepaired patients, surgical repair is indicated before preg of dissection. Spontaneous vaginal delivery is preferred with use of epi pregnancy have been reported in up to 12% of patients. Pre women with marked dilatation of the right ventricle due to pregnancy relief of stenosis (usually by balloon valvuloplasty) severe pulmonary regurgitation, pre-pregnancy pulmonary valve should be performed in severe stenosis (peak Doppler gradient 19 19,68,105 replacement (homograft) should be considered. Severe pulmonary regurgitation has been identied as an inde Obstetric and offspring risk pendent predictor of maternal complications, especially in patients 76,106 the risk of offspring complications is increased. Follow-up every trimester is sufficient in the majority of prosthesis) should be considered. In women with severe pulmonary regurgitation, monthly or bimonthly cardiac evaluation with echocardiography is indi Obstetric and offspring risk cated. Transcatheter valve hypertension-related disorders including (pre-)eclampsia, may be implantation or early delivery should be considered in those 103 who do not respond to conservative treatment. The incidence of offspring compli 103 cations also appears to be higher than in the general population. The preferred mode of delivery is vaginal in almost all Pulmonary regurgitation generally carries no additional offspring cases. The incidence of arrhythmias may rise during preg have an increased risk of developing complications such as arrhyth nancy and is associated with a worse prognosis. Women with Ebsteins anomaly and interatrial shunting can develop shunt reversal and cyanosis in pregnancy. There is also a risk of paradoxical emboli (see Obstetric and offspring risk Section 3. Maternal risk Though many women tolerate pregnancy relatively well, after an Delivery.
Blackhaw (Black Haw). Clonidine.
- Are there safety concerns?
- How does Black Haw work?
- What is Black Haw?
- Dosing considerations for Black Haw.
- Diarrhea, increasing urine, preventing miscarriage, asthma, menstrual cramps, spasms of the uterus (womb) following childbirth, and other conditions.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=96859
Cheap clonidine 0.1 mg visa
Discharge Date (A2000 on existing record to be modified/inactivated Complete only if X0600F = 10 blood pressure and exercise generic clonidine 0.1mg on-line, 11, or 12. Altered Level of Consciousness Did the resident have altered level of consciousness, as indicated by fluctuate. Say to resident: "Over the last 2 weeks, have you been bothered by any of the following problems Activity did not occur activity did not occur or family and/or non-facility staff provided Self-Performance. Locomotion on unit how resident moves between locations in his/her room and adjacent corridor on same floor. Toilet use how resident uses the toilet room, commode, bedpan, or urinal; transfers on/off toilet; cleanses self after elimination; changes pad; manages ostomy or catheter; and adjusts clothes. Do not include emptying of bedpan, urinal, bedside commode, catheter bag or ostomy bag. Helper lifts, holds, or supports trunk or limbs, but provides less than half the effort. Lower body dressing: the ability to dress and undress below the waist, including fasteners; does not include footwear. Car transfer: the ability to transfer in and out of a car or van on the passenger side. Walk 10 feet: Once standing, the ability to walk at least 10 feet in a room, corridor, or similar space. Setup or clean-up assistance Helper sets up or cleans up; resident completes activity. Walking 10 feet on uneven surfaces: the ability to walk 10 feet on uneven or sloping surfaces (indoor or outdoor), such as turf or gravel. Picking up object: the ability to bend/stoop from a standing position to pick up a small object, such as a spoon, from the floor. Frequently incontinent (7 or more episodes of urinary incontinence, but at least one episode of continent voiding). Injury (except major) skin tears, abrasions, lacerations, superficial bruises, hematomas and 2. Stage 2: Partial thickness loss of dermis presenting as a shallow open ulcer with a red or pink wound bed, without slough. Moderately impaired limited vision; not able to see newspaper headlines but can identify objects. How resident takes full-body bath/shower, sponge bath, and transfers in/out of tub/shower (excludes washing of back and hair). Activity itself did not occur or family and/or non-facility staff provided care 100% of the time for that activity over the entire 7-day period. Indicate the residents usual ability with everyday activities prior to the current illness, exacerbation, or injury. Indicate devices and aids used by the resident prior to the current illness, exacerbation, or injury. Wheel 50 feet with two turns: Once seated in wheelchair/scooter, the ability to wheel at least 50 feet and make two turns. Darkly pigmented skin may not have a visible blanching; in dark skin tones only it may appear with persistent blue or purple hues. Application of nonsurgical dressings (with or without topical medications) other than to feet. Enter Days Record the number of days that injections of any type were received during the last 7 days or since admission/entry or reentry if less than 7 days. Check all of the following treatments, procedures, and programs that were performed during the last 14 days. If the sum of individual, concurrent, and group minutes is zero, skip to O0400A5, Therapy start date Enter Number of Minutes 3A. Days record the number of days this therapy was administered for at least 15 minutes a day in the last 7 days. Record the number of days each of the following restorative programs was performed (for at least 15 minutes a day) in the last 7 calendar days (enter 0 if none or less than 15 minutes daily). Does the resident (or family or significant other or guardian or legally authorized representative if resident is unable to understand or respond) want to be asked about returning to the community on all assessments No referral is or may be needed (For more information see Appendix C, Care Area Assessment Resources #20). Chair/bed-to-chair transfer: the ability to transfer to and from a bed to a chair (or wheelchair). Number of these Stage 4 pressure ulcers that were present upon admission/entry or reentry enter how many were noted at the time of admission/entry or reentry. Number of unstageable pressure ulcers/injuries due to non-removable dressing/device If 0 Skip to M0300F, Unstageable Slough and/or eschar. Number of unstageable pressure injuries presenting as deep tissue injury If 0 Skip to N2005, Medication Intervention. Entry Date (A1600 on existing record to be modified/inactivated) Complete only if X0600F = 01. Enter Code Hearing aid or other hearing appliance used in completing B0200, Hearing. Usually understood difficulty communicating some words or finishing thoughts but is able if prompted or given time. Behavior continuously conversation, unclear or illogical flow of ideas, or unpredictable switching from subject to subject) Enter Score Add scores for all frequency responses in Column 2, Symptom Frequency. Indicating that s/he feels bad about self, is a failure, or has let self or family down. Hallucinations (perceptual experiences in the absence of real external sensory stimuli). Independent Resident completed the the toilet, or eating prior to the current illness, exacerbation, or injury. Dependent A helper completed the activities or without a device such as cane, crutch, or walker) prior to the current illness, for the resident. Supervision or touching assistance Helper provides verbal cues and/or touching/steadying and/or contact guard assistance as resident completes activity. Hip Fracture any hip fracture that has a relationship to current status, treatments, monitoring. Diagnoses listed in parentheses are provided as examples and should not be considered as all-inclusive lists. Enter Rating Ask resident: "Please rate your worst pain over the last 5 days on a zero to ten scale, with zero being no pain and ten as the worst pain you can imagine. Enter Code Ask resident: "Please rate the intensity of your worst pain over the last 5 days. Did the resident have a fall any time in the last month prior to admission/entry or reentry Did the resident have any fracture related to a fall in the 6 months prior to admission/entry or reentry Proportion of total calories the resident received through parenteral or tube feeding. Broken or loosely fitting full or partial denture (chipped, cracked, uncleanable, or loose). Number of Stage 4 pressure ulcers If 0 Skip to M0300E, Unstageable Non-removable dressing/device. Number of these unstageable pressure injuries that were present upon admission/entry or reentry enter how many were noted at the time of admission/entry or reentry. Identification of Record to be Modified/Inactivated the following items identify the existing assessment record that is in error. Enter Number Enter the number of correction requests to modify/inactivate the existing record, including the present one.
Cheap clonidine 0.1mg fast delivery
This includes obtaining food and utensils within the home blood pressure numbers low 0.1mg clonidine with amex, opening packages, and other necessary preparation such as pouring, mixing or warming; does not include grocery shopping or main meal preparation. This includes locating phone numbers, dialing the correct number, and communicating by phone. This includes washing/drying dishes, dusting, making their bed, or taking care of their belongings, in the home. Includes sorting, washing, or folding laundry either in or outside the home; does not include transportation. For example, when discussing arranging shopping with a caregiver, be sure to inquire specifically how the resident remembers what items are needed, specifies their brand, size, or color preferences, and notifies others of the need for shopping assistance. The wording used in each coding option is intended to reflect real-world situations in residential care facilities, where slight variations are common. For example, a resident may be independent in arranging Transportation for routine daily activities, but may require assistance for arranging transportation for evening outings (such as assistance with reading evening bus schedules). In this case, on Arranging Transportation, the resident self-performance would be coded 1 (Done with Help). There are many possible reasons for these variations, including mood, medical condition, relationship issues and medications. Talk with staff from day and evening shifts to ascertain what the resident does for himself or herself relative to transportation. Residents who have difficulty getting between buildings and vehicles, or who have difficulty locating their destination are distinguished based on their need for assistance beyond simply driving a vehicle. For example, a resident may be able to drive to local shopping areas for routine activities, but may require someone else to drive them to appointments that are out of town and escort them into unfamiliar buildings to locate a new doctors office. Individual accompanying resident may have supervised resident by observing that resident managed to safely gain access to the destination building. Even if highly independent in an activity, the resident may believe he or she can do better. Process: Ask if the resident thinks he or she could be more self-sufficient given more time assistive devices, or training/therapy. New Devices Needed Intent: To determine whether the resident needs new or additional assistive devices and what if any, is needed. A complete denture replaces all of the teeth; a partial denture replaces some teeth. If the resident expresses or gives evidence of needing an assistive device that is not listed, check box lettered g for Other and specify the device. Research has shown that 14 days are the minimum to obtain an accurate picture of bowel continence patterns. For the sake of consistency, both bowel and bladder continence are evaluated over 14 days. Make sure that your discussions are held in private as control of bladder and bowel functions are sensitive subjects, particularly for residents who are struggling to maintain control. Many people with poor control will hide their problems out of embarrassment or fear of retribution. Others will not report problems to staff because they mistakenly believe that incontinence is a natural part of aging and nothing can be done to reverse the problem. Despite these common reactions to incontinence, many elders are relieved when a health care professional shows enough concern to ask about the nature of the problem in a sensitive and straightforward manner. Remember to consider continence patterns over the last 14-day period, 24 hours a day, including weekends. If staff assignments change frequently, consider initiating and maintaining a bladder and bowel elimination flow sheet in order to gather more accurate information. Coding: Choose one response to code the level of bladder continence and one response to code level of bowel continence for the resident over the last 14 days. Do not record the level of control that the resident might have achieved under optimal conditions. Notice that in each category, different frequencies of incontinent episodes are specified for bowel and bladder. The reason for these differences is that there are more episodes of urination per day and week, compared to bowel movements, which typically occur less often. Q was taken to the toilet after every meal, before bed, and once during the night. Although she is generally continent of urine, every once in a while (about once in two weeks) Mrs. Review the record, particularly any documentation flow sheets of bowel elimination patterns. Bladder retraining program A retraining program where the resident is taught to consciously delay urinating (voiding) or resist the urgency to void. Residents are encouraged to void on schedule rather than according to their urge to void. This form of training is used to manage urinary incontinence due to bladder instability. Indwelling catheter A catheter that is maintained within the bladder for the purpose of continuous drainage of urine catheters inserted through the urethra or by supra-pubic incision.
Order 0.1mg clonidine overnight delivery
With an autosomal recessive condition blood pressure medication that doesn't cause ed generic 0.1mg clonidine with amex, the full siblings of the affected individual have a 25% chance of being affected, a 50% chance of being an unaffected carrier, and a 25% chance of being neither a carrier nor affected. Item C168 denotes autosomal recessive inheritance recurrence risk for a couple who are both carriers of a disorder to have another affected child (1 in 4 risk). In addition to cystic fibrosis, other types of autosomal recessive conditions commonly encountered in pediatrics include sickle cell disease, phenylketonuria, galactosemia, and other inborn errors of metabolism. The remaining answer choices (0%, 33%, 50%, 75%) would be incorrect with regards to recurrence risk for a future sibling given 2 presumed carrier parents. If a child had an autosomal dominant condition, such as Marfan syndrome, inherited from an affected parent, the risk would be 50% for the childs future siblings as well as for the childs offspring later in life. Cystic fibrosis population carrier screening: 2004 revision of American College of Medical Genetics mutation panel. Preparing for the encounter, you briefly review pubertal growth and development in boys and its assessment. The earliest sign of puberty in 98% of boys is an increase in testicular volume to 4 mL or more, or 2. The average age at which testicular enlargement (gonadarche) begins is 10 years in non-Hispanic white boys, 9 years in black boys, and 10 years in Hispanic boys, respectively. Unlike in girls, precocious puberty is rare in boys and may be due to a pathologic cause that requires evaluation. When it occurs very early or is rapidly progressive, treatment is recommended to preserve adult height and address psychosocial concerns. He had tympanostomy (pressure-equalizing) tubes placed by an otolaryngologist when he was 18 months of age because of chronic middle ear effusion with hearing loss. Today, you clearly visualize a blue tympanostomy tube in his left tympanic membrane. His right tympanic membrane appears normal with no tympanostomy tube and no evidence of perforation. The risks of tympanostomy tube insertion include anesthesia-related risks and tympanic membrane damage, including otorrhea, tympanosclerosis, focal atrophy, or persistent perforation. Most tympanostomy tubes placed in the United States are designed to remain in place for a short time, typically 12 to 18 months. Over time, as the epithelial layer of the tympanic membrane turns over, most tubes are spontaneously extruded. Tympanostomy tubes that remain in place for longer than 3 years are unlikely to spontaneously extrude; they are more likely to lead to chronic tympanic membrane perforation. Yearly examinations are not appropriate because the remaining tube is unlikely to spontaneously extrude. Neither irrigation of the ear canal nor corticosteroid otic drops induce extrusion. They are also indicated for children with recurrent acute otitis media who have middle ear effusion at the time of assessment. Rate of persistent perforation after elective tympanostomy tube removal in pediatric patients. She has undergone multiple palliative cardiac surgical procedures, and her cardiac care team has communicated to you that there is no other procedure or intervention that can be performed. You refer her to the emergency department for further evaluation and management of a presumed cerebrovascular accident. Among heart failure, iron deficiency anemia, polycythemia, pulmonary overcirculation, and viral illness, the most likely predisposing factor is the polycythemia seen in patients with chronic cyanosis. Patients with congenital heart disease are more likely to survive and live longer than ever before. Many therapies, procedures, and operations for congenital heart disease are palliative (not curative). Complications are relatively common and increase in prevalence and severity as patients age. It is important to understand the associated long-term effects and complications of congenital heart disease. Complications, such as heart failure caused by systolic dysfunction, diastolic dysfunction, valve regurgitation, and stenosis, can lead to symptoms such as fatigue, exercise intolerance, shortness of breath, anorexia, and vomiting. Arrhythmias are common and can result in symptoms of heart failure as well as the perception of a fast or slow heartbeat, dizziness, palpitations, or syncope. Pulmonary hypertension can lead to pulmonary hemorrhage, syncope, and heart failure. Patients are also at risk for other organ injury such as hepatic and renal disease. Neurologic problems are common and include cognitive delay, attention-deficit disorder, and cerebrovascular accidents, as described for the patient in this vignette. One reason for these thromboembolic events is the polycythemia that occurs in chronically cyanotic patients, such as the patient in this vignette. Iron deficiency anemia and viral illness are not described in this vignette and are not specifically associated with congenital heart disease. Pulmonary over circulation and heart failure can occur in congenital heart disease but are unlikely to cause the neurologic symptoms seen in the patient in this vignette. Polycythemia in the setting of chronic cyanosis increases the risk of a thromboembolic event. Many patients with cyanotic congenital heart disease are treated prophylactically with aspirin, warfarin, or other anticoagulants to help prevent thromboembolic events. Consultation with the specialist: complications of polycythemia in patients who have cyanotic congenital heart disease. Results of a urine test strip analysis are shown: Laboratory Test Result Specific gravity 1. Based on your findings, you suspect acute postinfectious glomerulonephritis as the underlying cause of the patients symptoms. Systemic lupus erythematosus is a chronic inflammatory disease with multisystem involvement that may include skin, joints, kidneys, lungs, nervous system, serosal membranes, or other organs. Systemic lupus erythematosus in children may present with renal involvement alone. The renal involvement may manifest as hematuria and proteinuria identified on routine examination, nephrotic syndrome (proteinuria, edema, and hypoalbuminemia), or acute nephritis (acute renal failure, hematuria, and hypertension). Acute poststreptococcal glomerulonephritis: the most common acute glomerulonephritis. She ran head-on into a brick wall and then fell from her bicycle onto the sidewalk. The girls friends report that she lost consciousness briefly (<1 minute) after hitting the wall, but then was crying and asking them to call her mother. Paramedics found the avulsed teeth on the sidewalk at the scene of the accident, which they transported to the emergency department in a plastic bag. She seems uncomfortable, but is answering questions appropriately and following directions. The girls airway is intact, and she is breathing easily with equal breath sounds. She has a 5-cm hematoma in the center of her forehead, with abrasion of the overlying skin and multiple abrasions to her face. There is dried blood in both of her nares, but no deformity of her nasal bridge and there is no septal hematoma. There is a 1-cm laceration to the inner surface of her lower lip, which appears fairly deep but does not cross the vermilion border. Both of her upper central incisors are missing, with small blood clots at both tooth sockets. All pediatric providers should be familiar with the appropriate management of an avulsed tooth. Avulsed permanent teeth should be immediately reimplanted, as the prognosis is best when reimplantation is completed within 15 to 30 minutes of avulsion. Patients/parents/bystanders should be encouraged to replace an avulsed tooth into its socket as soon as possible. Children can bite on a cloth/handkerchief to hold the tooth in position until they can access dental care.
Clonidine 0.1mg without a prescription
Adverse effects most commonly reported in adults and children are pain at the injection site hypertension 12080 purchase 0.1 mg clonidine, reported by 3% to 29% of recipients, and a temperature greater than 37. Anaphylaxis is uncom mon, occurring in approximately 1 in 600 000 recipients, according to vaccine adverse events passive reporting surveillance systems. No adverse effect on the developing fetus has been observed when pregnant women have been immunized. Susceptibility testing before immunization is not indicated routinely for children or adolescents. Postimmunization testing also should be considered in people 65 years of age or older. Fewer than 5% of immunocompetent people receiving 6 doses of hepatitis B vaccine adminis tered by the appropriate schedule in the deltoid muscle fail to develop detectable antibody. However, few data exist con cerning the response to higher doses of vaccine in children and adolescents, and no specifc recommendations can be made. For people with progressive chronic renal failure, hepatitis B vaccine is recommended early in the disease course to provide protection and potentially decrease the need for larger doses once dialysis is initiated. Hepatitis B immu nization is recommended for all infants, children, and adolescents through 18 years of age. Delivery hospitals should develop policies and procedures that ensure administration of a birth dose as part of the routine care of all medically stable infants weighing 2000 g or more at birth, unless there is a physicians order to defer immunization and a report of the negative serologic status of the mother is in the infants medical record. Only single-antigen hepatitis B vaccine can be used for doses given between birth and 6 weeks of age. For guidelines for mini-1 mum scheduling time between vaccine doses for infants, see Table 1. The schedule should be chosen to facilitate a high rate of adherence to the primary vaccine series. For immunization of older children and adolescents, doses may be given in a schedule of 0, 1, and 6 months; of 0, 1, and 4 months; or of 0, 2, and 4 months (although shorter intervals between frst and last doses result in lower immunogenicity). For older children and ado lescents, spacing at 0, 12, and 24 months results in equivalent immunogenicity and can be used when an extended administration schedule is acceptable on the basis of low risk of exposure. A 2-dose schedule for one vaccine formulation is licensed for people 11 through 15 years of age; the schedule is 0 and then 4 to 6 months later (see Table 3. Children and adolescents who previously have not received hepatitis B vaccine should be immunized routinely at any age with the age-appropriate doses and schedule. Selection of a vaccine schedule should consider the need to achieve completion of the vaccine series. In all set tings, immunization should be initiated even though completion of the vaccine series might not be ensured. Hepatitis B immunization may be admin-1 istered at the discretion of the treating clinician to unimmunized adults with diabetes mellitus who are 60 years of age or older. For infants, children, adolescents, and adults with lapsed immu nizations (ie, the interval between doses is longer than that in one of the recommended schedules), the vaccine series can be completed, regardless of the interval from the last dose of vaccine (see Lapsed Immunizations, p 35). Studies demonstrate that decreased seroconversion rates might occur among certain preterm infants with low birth weight (ie, less than 2000 g) after administration of hepatitis B vaccine at birth. However, by the chronologic age of 1 month, all medically stable preterm infants (see Preterm and Low Birth Weight Infants, p 69), regardless of initial birth weight or gestational age, are as likely to respond to hepati this B immunization as are term and larger infants. For information on use of combination vaccines containing hepatitis B vaccine as a component to complete the series, see Table 3. Considerations for High-Risk Groups: Health Care Professionals and Others With Occupational Exposure to Blood. Health care professionals who have contact with blood or other poten tially infectious body fuids should be immunized. Immunization early in the course of renal disease is encouraged, because response is better than in advanced disease. Specifc dosage rec ommendations have not been made for children undergoing hemodialysis. Some experts recommend increased doses of hepatitis B vaccine for children receiving hemodialysis to increase immunogenicity. Unimmunized or underimmunized people in juvenile and adult correctional facilities should be immunized. If the length of stay is not suffcient to complete the immunization series, the series should be initiated and follow-up mechanisms with a health care facil ity should be established to ensure completion of the series (see Hepatitis and Youth in Correctional Settings, p 186). Immunization should begin at least 4 to 6 months before travel so that a 3-dose regimen can be completed (see Preexposure Universal Immunization, p 380). If immunization is ini tiated fewer than 4 months before departure, the alternative 4-dose schedule of 0, 1, 2, and 12 months, licensed for one vaccine (see Table 3. Individual clinicians may choose to use an accelerated schedule (eg, doses at days 0, 7, and 21) for travelers who will depart before an approved immunization schedule can be completed. Studies are limited on the maximum interval after exposure during which postexposure prophylaxis is effective, but the interval is unlikely to exceed 7 days for percutaneous exposures and 14 days for sexual exposures. All pregnant women should be tested during an early prenatal visit with every pregnancy. For infants who weigh less than 2000 g at birth, the initial vaccine dose should not be counted in the required 3-dose schedule (a total of 4 doses of hepatitis B vaccine should be admin istered), and the subsequent 3 doses should be given in accordance with the schedule for immunization of infants weighing <2000 g (see Preterm and Low Birth Weight Infants, p 69). In these infants, the initial vaccine dose should not be counted toward the 3 doses of hepatitis B vaccine required to complete the immunization series. Postexposure Prophylaxis for People With Discrete Identifable Exposures to Blood or Body Fluids. Immunization is recommended for any person who was exposed but not previously immunized. The vaccine series should be completed using an age-appropriate dose and schedule. Children and adolescents who have written documentation of a complete hepatitis B vaccine series and who 1Centers for Disease Control and Prevention. Children and adolescents with written documentation of a complete hepatitis B vaccine series require no further treatment (Table 3. For unimmunized victims of sexual assault or abuse, active postexposure prophylaxis (ie, vaccine alone) should be initiated, with the frst dose of vaccine given as part of the initial clinical evaluation. All children, including children who attend child care, should receive hepa titis B vaccine as part of their routine immunization schedule. The Centers for Disease Control and Prevention Division of Viral Hepatitis main tains a Web site ( Acute disease tends to be mild and insidious in onset, and most infections are asymptomatic. Jaundice occurs in fewer than 20% of patients, and abnormalities in liver transaminase concentrations generally are less pronounced than abnormalities in patients with hepa titis B virus infection. Although chronic hepatitis develops in approxi mately 70% to 80% of infected adults, limited data indicate that chronic hepatitis and cirrhosis occur less commonly in children, in part because of the usually indolent nature of infection in pediatric patients. Seroprevalences vary among populations according to their associated risk factors. The most common risk factors for acquiring infection are injection drug use, having mul tiple sexual partners, or having received blood products before 1992. Also, more recently appreci ated has been the number of infections acquired in the health care setting, especially nonhospital clinics, in which infection control and needle and intravenous hygienic procedures have not been strict. Transmission among family contacts is uncommon but can occur from direct or inapparent percutaneous or mucosal exposure to blood. Seroprevalence among pregnant women in the United States has been estimated at 1% to 2%. Third-generation enzyme immunoassays are at least 97% sensitive and more than 99% specifc. However, false-positive and false-negative results can occur from improper handling, stor age, and contamination of test specimens. The clinical value of these quantitative assays appears to be primarily as a prognostic indicator for patients undergoing or about to undergo antiviral therapy.
Purchase genuine clonidine on-line
If there has been more than one minutes after the reaction has entirely extension blood pressure medication raises pulse cheap clonidine 0.1 mg free shipping, the O2 breathing at 30 feet is subsided and resume schedule at point of increased to 60 minutes. Table 6 can be lengthened up to 2 additional an additional 60-minute O2 period is taken at 25-minute periods at 60 feet (20 minutes on 30 feet. Ascent rate 165 fsw to 60 fsw not to exceed 3 ft/min, 60 fsw and shallower, not to exceed 1 ft/min. If initial treatment was at 60 feet, up to 20 minutes may be spent at 60 feet before compression to 165 fsw. If a chamber is equipped with a high-O2treatment gas, it may be administered at 165 fsw and shallower, not to exceed 2. Table 6A can be lengthened up to 2 additional 25-minute periods at 60 feet (20 minutes on oxygen and 5 minutes on air), or up to 2 additional 75-minute periods at 30 feet (60-minutes on oxygen and 15 minutes on air), or both. Tenders breathes 100 percent O2during the last 60 minutes at 30 fsw and during ascent to the surface for an unmodified table or where there has been only a single extension at 30 or 60 fsw. If there has been more than one extension, the O2breathing at 30 fsw is increased to 90 minutes. If the tender had a hyperbaric exposure within the past 12 hours, an additional 60 minute O2breathing period is taken at 30 fsw. If significant improvement is not obtained within 30 minutes at 165 feet, consult with a Diving Medical Officer before switching to Treatment Table 4. If initial treatment has progressed to a depth shallower than 60 feet, compress to 60 feet at 20 ft/min to begin Table 7. Remain at 60 feet a minimum of 12 hours unless overriding circumstances dictate earlier decompression. Ensure chamber life-support requirements can be met before committing to a Treatment Table 7. A Diving Medical Officer shall be consulted before committing to this treatment table. As ambient atmospheric pressure decreases with increased altitude, partial pressures of oxygen also drop. See also related injuries such as acute mountain sickness, high altitude pulmonary edema, high altitude cerebral edema hypoxia associated with diving. Subjective: Symptoms Variable from person to person, but consistent in an individual across exposures; impaired judgement, thinking, and vision (particularly color vision); paresthesias, especially of the face and hands, are common. Assessment: Resolution of signs and symptoms with return to lower altitudes or treatment with oxygen confirms the diagnosis. Alternative: Increase oxygen concentration of inspired air by any other means (different masks, etc. Primitive: Increase ambient pressure by decreasing altitude or adjusting cabin altitude 6-31 6-32 Patient Education General: Effects of hypoxia are experienced only while exposed to a hypoxic environment. Patient will likely be affected in similar manner by exposure to similar altitudes. Prevention: Early recognition of the symptoms of hypoxia allows early intervention and avoids performance decrement. Use pre-mission altitude chamber testing to determine individual team members response to the hypobaric environment. There is tremendous opportunity for impairment of judgement and thinking, which can quickly lead to death or serious injury. Hypoxia may also manifest less acutely in association with living and working at high altitude. An acute hypoxic event without complications or sequelae is not grounds for restriction of special duty status. When the ambient pressure changes, the pressure differential in the trapped pocket of gas cannot be equalized and severe pain results. Since barodontalgia may develop during diving or flight operations, see also Dive Medicine chapter. Subjective: Symptoms Acute onset of sharp, stabbing pain in a single tooth on ascent. This pain can be quite severe and will increase in severity with continued ascent. Assessment: History makes the diagnosis, especially in a patient with risk factors. Consider fracture of tooth or removal/replacement of restoration if symptoms are unrelenting in an operational setting that precludes descent. Patient Education General: Whenever possible do not fly while suffering from acute dental disease. Follow-up Actions Return evaluation: Dental exam for diagnosis and treatment of underlying pathology. Consultation Criteria: For severe cases, when symptoms not relieved upon descent, or when underlying pathology is the cause. The pressure within the sinuses is normally equal to ambient air pressure and equalizes as ambient pressure changes. When the pressure cannot be equalized due to malformations or swelling of the sinus outflow tract, pain results. This is more likely to occur when descent from altitude results in a sinus "squeeze. Subjective: Symptoms Acute onset of sharp, stabbing sinus pain on descent is classic. Symptoms will abate with decreasing ambient pressure resulting from return to altitude. Patients will bleed into the sinus in severe cases, thereby relieving the pressure differential and significantly reducing the pain. Some redness and swelling of the face in the affected area may be noted though not to the degree one would expect with purulent sinusitis. Using Advanced Tools: X-ray: Sinus series X-rays (looking for air/fluid levels) are helpful if available. Assessment: Differential Diagnosis Barodontalgia caused by air trapped under a crown or amalgam or within a tooth cavity; may be suggested by maxillary sinus symptoms present on ascent Pulpitis or periapical abscess of the tooth if maxillary sinus symptoms associated with a diseased tooth are present on ascent 6-33 6-34 Acute infectious sinusitis may be indicated if systemic symptoms and/or purulent discharge is present Plan Treatment Primary: Increase cabin altitude to decrease pressure differential in sinus and alleviate pain. Patient Education General: It is easier to prevent a sinus "squeeze" than to treat one. Use modified Valsalva maneuver to equalize pressure in sinuses frequently during descent; do not wait until pain develops to attempt to equalize. Follow-up Actions Return evaluation: Patient should be followed and nasal decongestants (po or topical) should be used for several days following an episode of barosinusitis. If sinus bleeding occurs, treat with amoxicillin (250 mg po tid) and manage like acute sinusitis. The pressure within the middle ear is normally equal to the ambient pressure and equalizes through the Eustachian tube as ambient pressure changes. Pain results when the pressure cannot be equalized due to malformations or swelling of the Eustachian tube. Both conditions are more likely to occur with descent, but a reverse "squeeze" can occur on ascent with similar symptoms. As barotitis may develop during both diving or flight operations, see Dive Medicine chapter also. Subjective: Symptoms Acute onset of sharp, stabbing pain in the ear on descent is classic. This pain can be quite severe and will increase in severity with continued descent. Plan: Treatment Primary: Change cabin altitude to decrease pressure differential and alleviate pain (increase altitude if symptoms presented on descent, or vice versa). Use a Politzer bag, a device similar in appearance to an Ambu bag (and often carried on medical evacuation aircraft), to force air into the nasopharynx while the patient swallows. Primitive: Modified Valsalva maneuver (as above) Patient Education General: It is easier to prevent an ear "block" than to treat one. Use modified Valsalva maneuver to equalize pressure in middle ear frequently during descent; do not wait until pain develops to attempt to equalize. Prevention: Whenever possible, do not fly while suffering from an upper respiratory infection. Follow-up Actions Return evaluation: Patient should be followed and decongestants (po or nasal) should be used for several days following an episode of barotitis. Diffuse mottling of skin or central neurologic signs may indicate arterial gas embolism and are ominous. Examiner must perform a complete neurologic examination, to include mental status exam (see Appendix).

