Seroquel
Purchase 200 mg seroquel free shipping
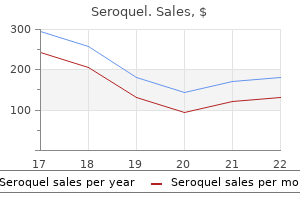
In order to inform the increasingly complex patient discussions around management of a papilloma without atypia diagnosed by core biopsy treatment h pylori 300 mg seroquel with mastercard, it is important to examine our institutional upgrade rate from papilloma on needle core biopsy to atypia or malignancy on excisional biopsy. Any patient with the diagnosis of intraductal papilloma by core biopsy who underwent excision were included in the study. The clinical manifestations and radiographic characteristics were recorded for correlation with final diagnosis by excision. Results: There were 87 patients with benign intraductal papilloma without atypia on core biopsy that underwent excisional biopsy. Conclusions: Management of benign papilloma diagnosed by core biopsy requires nuanced decision making and should give consideration to patient risk aversion. Based on our study results, we can counsel patients with intraductal papilloma without atypia and concordant imaging that the risk of delayed cancer diagnosis at our institution is quite low. Patients who would consider increased surveillance or chemoprophylaxis in light of a diagnosis of atypia may benefit from excision of a papilloma. The procedures were done under real-time ultrasound monitoring of ice ball formation. Conclusions: Using office-based cryoablation for the treatment of benign breast lesions is safe and cost effective. A retrospective review of 2,120 total core-needle biopsies performed over 60 months at our community hospital was conducted. Of those patients with upgrade, 7 were English-speakers or had unknown primary language, 4 spoke Chinese, and there were 1 of each of the following languages: Polish, Bengali, Spanish, Korean, and Farsi/Persian. Two patients had a known first-degree relative with breast cancer, and 9 patients initially presented with an abnormal mammogram, while 3 patients noticed a palpable mass prompting evaluation. No true local recurrences were found; 1 patient had local recurrence suspected on mammogram, but biopsy was consistent with radial scar and sclerosing papilloma instead. This study met its aims: it not only reflects, but also greatly broadens, the minimal prior literature demonstrating surgical approach with excisional biopsy and low recurrence rates with follow 198 up. Univariate and multivariate logistic regression was used to identify predictors of any wound problem (superficial, deep-space infections, dehiscence). Conclusions: Short-term post-operative complications after breast surgery are low. We have identified both modifiable and non-modifiable risk factors for the development of post-operative wound complications. Specifically, age less than 40, diabetes, obesity, smoking history, or reconstruction were predictive of post-operative wound complications. By identifying modifiable risk factors, practitioners can highlight the importance of blood sugar control, weight management, and smoking cessation to their patients. Future studies may look at outcomes following immediate versus delayed reconstruction as they relate to obesity, diabetes, and smoking history, which may help guide recommendations for the type of reconstruction best suited for each patient. Practitioners should be aware of and educate patients regarding the modifiable and non-modifiable risk factors for developing complications post-operatively. Patients with a unilateral diagnosis of invasive or in-situ cancer undergoing mastectomy were identified. Results: A total of 8378 women were included, with 4189 in each of the 2 balanced comparison groups. Rates of bleeding requiring transfusion were also higher in the bilateral mastectomy group (4. Between groups, there was no difference in respiratory, renal, cardiovascular, neurologic, urogenital or septic complications. Conclusions: this large multi-center study demonstrates that the addition of contralateral prophylactic mastectomy results in higher surgical complication rates, especially rates of wound infection and bleeding. Previous evidence suggests that growing awareness, availability, and access to immediate reconstructive surgery may influence the decision to pursue this more aggressive treatment. Methods: Purposive and snowball sampling strategies were used to recruit participants from academic and community hospitals across the province of Ontario, Canada. Plastic surgeons who perform reconstructive breast procedures participated in semi-structured one-on-one interviews that were audio recorded and transcribed verbatim. Results: Eighteen Ontario plastic surgeons participated in the study and data saturation was reached. Ten of the 18 participants were female, and 56% (10/18) came from academic hospitals. The probability of any ipsilateral breast recurrence for all 4 treatments is seen in the figure. If invasive recurrence is used as the endpoint, the 10-year probabilities of local invasive recurrence are as follows: mastectomy = 2. It allows the full course of radiation therapy to be delivered in a single session. This provides the starting point for patient treatment, and also tissue for biomarker analysis in window-of-opportunity design clinical trials. The remaining variables were excluded due to low clinical significance and also to eliminate multi-collinearity. We recorded the rate of upstaging to invasive carcinoma in the breast, as well as the pathological status of the sentinel node(s). Physician knowledge levels about recurrence risks after lumpectomy and mastectomy were high: 737 (78%) stated that the local recurrence risk at 10 years after lumpectomy without radiation was 10-30%, 817 (87. Statistical methods included cluster analyses, logistic, and Cox regression models. Methods: A retrospective database review from the Helen F Graham Cancer Center & Research Institute cancer registry was performed from 2006-2010. Conclusions: All patients with hypertension, diabetes, and/or metabolic syndrome have worse breast cancer-specific survival. Our study now demonstrates worse breast cancer-specific survival further supporting the need to focus on management and prevention of obesity and associated comorbidities to improve breast cancer-specific survival. Of those, 2388 had race, ethnicity, pathologic, and clinical staging available for assessment. Only 3% were non-white non-Hispanic, with American Indian as the third most common ethnicity followed by non-Hispanic Black, Asian, and Asian Indian. Six percent of patients in this cohort died between 2012 and 2016; of note, most of these patients were not diagnosed as Stage 4 at presentation (75%). Conclusions: Breast cancer patients in our hospital system present at higher stage of disease than the national average, with less cases of in situ cancers due to decreased screening. Methods: Women diagnosed with invasive breast cancer from 2001 to 2012 were identified in the Texas Cancer Registry (n=99,497). These patients received more therapies, but they had a significantly longer time to treatment as well as associated worse disease-specific survival. The literature suggests that racial and socioeconomic disparities exist in the incidence and survival of breast cancer. Results: There were 1139 (<1%) out of 411,001 patients who were recommended for surgery but had a surgical contraindication unrelated to their cancer. Conclusions: Racial, socioeconomic, and clinicopathologic disparities exist in the surgical treatment of breast cancer. Our aim was to determine whether the state-funded cancer care treatment program contributes to an improvement in mortality rate. Institutional differences were different across age, with older women more likely to undergo mastectomy at both community centers and integrated network cancer centers (Table). We sought to explore relationships between patient weight and breast cancer presentation and outcomes across cancer subtypes. Comparisons across categories were performed with Chi-squared analyses; non-parametric methodology was employed for continuous variables. Obese patients presented at higher pathologic stages for all cancer subtypes (p<0. Intense investigation is needed to unravel the interplay of genetic, epigenetic, and environmental factors that may be contributing to these observations. Studies have shown that cancer patients who file for bankruptcy have worse clinical outcomes than their financially solvent counterparts. Bivariate analysis comparing sociodemographic, clinical, and treatment variables between patients who filed for bankruptcy and those who did not was conducted. A logistic regression model was created to identify patients at increased risk of filing for bankruptcy after their diagnosis. A Cox regression model created on propensity score matching was used to determine the effect of filing for bankruptcy on 5-year all-cause mortality. Conclusions: Among Indiana breast cancer patients, younger age, residency in a high poverty area, no insurance at diagnosis, and regional disease at diagnosis increased the probability of filing for bankruptcy after a diagnosis of breast cancer.
Seroquel 50mg generic
Prevalence of nonpolypoid (flat and depressed) colorectal neoplasms in asymptomatic and symptomatic adults oxygenating treatment order 300mg seroquel otc. Single-stage treatment for malignant left-sided colonic obstruction: a prospective randomized clinical trial comparing subtotal colectomy with segmental resection following intraoperative irrigation. Effect of hospital caseload on long-term outcome after standardization of rectal cancer surgery at a national level. The benefit of leucovorin-modulated fluorouracil as postoperative adjuvant therapy for primary colon cancer: results from National Surgical Adjuvant Breast and Bowel Project protocol C-03. World Cancer Research Fund and American Institute for Cancer Research Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. Prophylactic oophorectomy in colorectal carcinoma: preliminary results of a randomized, prospective trial. For each disease type, the current literature is reviewed to provide an explanation of epidemiology, pathology, clinical presentation, diagnosis, staging, and issues regarding surgical and multimodality therapy. A description of the major arterial variations is beyond the scope of this chapter; however, an overview of relevant hepatic anatomy essential to the discussion of resection options for hepatic tumors is provided. On the basis of the portal segmentation, eight separate anatomical segments of the liver can be identified, first described by Couinaud in 1957. This predominantly portal segmentation of the liver provides the surgeon with an anatomical approach to the liver, such that any of the eight segments can be resected while preserving the vascular inflow, venous outflow, and biliary drainage of the remaining segments. The caudate lobe has highly variable biliary and portal anatomy, as well as its own venous drainage, with short veins draining directly into the vena cava. The right liver can be divided into the right anterior and posterior sectors, and the left liver divided into the lateral and medial sectors. The middle hepatic vein defines the main plane, or the division between the left and right livers, which is the plane defining the right or left hepatectomy resection lines. Surgical techniques, including the Glissonian approach or dissection along the fibrous sheath that surrounds the portal triads, may enable the surgeon to identify important elements of the anatomy intrahepatically, and thereby minimize the risk of injury to the remaining liver after resection of anatomical segments. Accordingly, the Brisbane 2000 International Conference was held to establish a consensus on terminology used for liver resection. For patients with tumor-related cholestasis or marked underlying liver disease, a 40% liver remnant is necessary to avoid cholestasis, fluid retention, and liver failure. However, inaccuracy may arise because the liver to be resected is often diseased, particularly in patients with cirrhosis or biliary obstruction. Hypertrophy occurs quite rapidly, and the normal liver can be reassessed by volumetry within 3 or 4 weeks. However, hypertrophy may occur more slowly in cirrhotics, diabetics, and patients with other types of chronic liver injury; therefore, an interval of 5 or 6 weeks may be required to achieve the desired degree of hypertrophy. After a short interval (median 9 days; range 5 to 28 days) patients undergo completion hepatectomy. The proposed benefits include early abdominal exploration for intra or extrahepatic disease that might preclude curative resection as well as a shortened interval of hypertrophy prior to resection. In general, 5-year survival is rare among patients who undergo resection for noncolorectal metastases to the liver. The exceptions are selected patients with neuroendocrine tumors, Wilms tumor, and to a lesser extent, renal cell carcinoma; 5-year survival rates of 40% to 70% have been reported after resection in these cases. Hepatic resection may also provide excellent palliation in selected patients with hormone-secreting neuroendocrine tumors. Epidemiology and Etiology Colorectal cancer represents the third most common type of cancer for both men and women in the United States, with an estimated incidence of 135,000 cases per year. Approximately 80% of the patients will have malignancies that are amenable to surgical cure, but approximately 20% of the resected cancers will recur within 5 years. Only 20% of these recurrences will be solely or predominantly in the liver, and fewer still will be amenable to surgical resection. It has been estimated that 15,000 to 20,000 patients per year are potential candidates for resection of their liver metastases. Specific recommendations with regard to response to chemotherapy are difficult to make, although progression of liver metastasis during systemic chemotherapy should prompt selection of alternate chemotherapy agents rather than hepatic resection due to the poor outcomes observed in these patients. The planned hepatic resection should encompass all metastases detectable on prechemotherapy imaging. Conversely, patients with imaging suggestive of viable tumor after preoperative chemotherapy may demonstrate evidence of a complete pathologic response at the time of resection. The use of fiducial markers in very small lesions may be considered prior to initiation of chemotherapy in order to preserve localization of the site of disease at the time of resection. Median size was 12 mm and 83% (N = 34) were located >10 mm deep within the liver parenchyma. After receipt of chemotherapy, nearly half (46%) disappeared on cross-sectional imaging. All were treated with resection (N = 31) or ablation (N = 10), and no local recurrences were identified at median follow-up of 14 months. In cases of bilateral disease, multistage approaches to surgery should be considered. Preoperative systemic chemotherapy can reduce the size and volume of tumors such that all tumor sites can be resected safely and provide long-term survival. At the second stage, major hepatectomy or extended hepatectomy removes all remaining disease. The safety and efficacy of this approach has been recently reported by Passot et al. The cumulative rate of major complications during the first and second stages was 15% with 3-year survival of 68%. Although this difference may be representative of patient selection to some degree, complete resection of disease is associated with an excellent outcome. Additional decision-making is necessary in the setting of synchronous liver metastases to determine the order of resection of the primary colorectal cancer and liver metastases. The complexity of the operation necessary to remove the primary tumor and the extent of hepatic resection required will affect decision making because the risk of adverse events from hepatic resection increases when the procedure is associated with extrahepatic surgery. Solitary, small, peripherally located lesions in a healthy, hemodynamically stable patient that can be excised adequately by nonanatomical resection or segmentectomy may be resected at the same time as the primary tumor. Lesions that are larger or that will require a major hepatic resection are best approached during a separate operation. We have found that this results in an earlier recovery due to the fact that infectious complications are less common following liver resection compared to resection of the colorectal primary. Additionally, we consider disease progression in the liver to be the greatest risk to the patient, which is eliminated with resection of the liver disease first. In the specific setting of synchronous liver metastases and rectal cancer, patients are most often treated with neoadjuvant chemotherapy and liver resection, followed by chemoradiation and then resection of the primary rectal cancer. Several modern studies have highlighted the improvement in survival over time with the use of improved operative techniques, anesthesia, patient selection, imaging, and chemotherapy. They demonstrated a significant increase in the rate of 5-year overall survival, which was 31% in the early group and 58% in the latter group, despite similar rates of perioperative morbidity and mortality. Most patients required a major resection (64% underwent a hemi-hepatectomy or extended hepatectomy), and nearly one-fourth of the patients required a procedure in addition to hepatic resection. Additionally, the 3 and 5-year overall survival rates were higher in the group with an optimal morphologic response ([82% and 74%] and [60% and 45%]; P < 0. The improved prognosis associated with an optimal morphologic response has also been validated in medical patients with advanced colorectal liver metastases not amenable to resection. One of the most widely quoted studies to outline prognostic factors is from Fong et al. These factors contribute to outcome in different degrees, and scoring of these factors is helpful in predicting prognosis after resection, but not in selecting patients for surgery. The notion that a 1-cm margin is necessary to ensure long-term survival has been dispelled. Analysis of nearly 500 patients in a multi-institutional database showed that the pattern and probability of disease recurrence and the rates of disease-free and overall survival were identical in patients with 1-mm and 1-cm resection margins.
Syndromes
- Death
- Being very old or very young
- Bleeding from your rectum
- Lower gastrointestinal (GI) bleeding
- Infection
- Major depression
- Cognitive behavioral therapy (CBT)
- Special care of the pins or screws holding the device is needed to prevent infection.
Buy cheap seroquel 100mg online
There are a number of machines designed to provide continuous feedback to the surgeon regarding the degree of negative fluid balance medicine game buy seroquel 100mg cheap. The risk of fluid overload is reduced by the judicious restriction of intravenous fluid by the anesthesiologist. The administration of an appropriate dose of furosemide should be considered, and the surgeon should plan for the expeditious completion of the procedure. Excessive circulating sorbitol may cause hyperglycemia, and large volumes of glycine may elevate levels of ammonia in the blood (218). Media Delivery Systems Syringes can be used for office diagnostic procedures and are especially good for infusing dextran solution. The syringe can be operated by the surgeon and is either connected directly to the sheath or attached by connecting tubing. A pressure cuff may be placed around the infusion bag to elevate the pressure in the system. Caution must be exercised because this technique causes increasing extravasation if intrauterine pressure rises above the mean arterial pressure. A variety of infusion pumps are available, ranging from simple devices to instruments that maintain a preset intrauterine pressure. Simple pump devices continue to press fluid into the uterine cavity regardless of resistance, whereas the pressure-sensitive pumps reduce the flow rate when the preset level is reached, thereby impeding the efflux of blood and debris and compromising the view. Flexible hysteroscopes are self-contained in that they do not require a sheath; the single integrated channel is used to transmit gas or fluid to the endometrial cavity for distention. As a result, these instruments are generally of smaller diameter than rigid systems. Flexible hysteroscopes utilize fiberoptic bundles rather than lenses to transmit the image to the observer and, consequently, have lower resolution than rigid instruments of a similar diameter and typically do not have a channel with a caliber suitable for most hand instruments. The most commonly used hysteroscopes are 3 to 4 mm in diameter, although those using fibers can be smaller than 2 mm in diameter. Rigid endoscopes require an angled (fore-oblique) lens to provide the angled view useful for operative hysteroscopy and are available in 0-degree, 12 to 15-degree, and 25 to 30-degree models (Fig. The 0-degree telescope provides a panoramic view and is best for diagnostic procedures. Hysteroscopes with 25 to 30-degree angles are most often used for cannulation of the fallopian tubes or placement of sterilization devices, whereas 12 to 15-degree designs are a suitable compromise useful for diagnosis and ablation or resection. The utility of endoscopes with larger fore-oblique views may be offset by the tendency of resectoscopic electrodes to leave the visual field on full extension. Light Sources and Cables Adequate illumination of the endometrial cavity is essential. Because it runs from a standard 110 or 220-volt wall outlet, the light source requires no special electrical connections. For most cameras and endoscopes, the element must have at least 150 watts of power for direct viewing and preferably 250 watts or more for video and operative procedures (219). Video Imaging Although diagnostic hysteroscopy may be performed with direct visualization, it is best to use video guidance for prolonged operations. The camera must be sensitive because of the narrow diameter of the endoscope and the frequently dark background of the endometrial cavity, particularly when it is enlarged (Fig. Image Documentation A small video camera can be used to teach and to coordinate the procedure with the operating room team. It allows the acquisition of still or video images for future reference or teaching. When a video recorder is used, the camera should be attached directly to the recorder to preserve the image quality. A number of video recording formats are available, each with inherent advantages and disadvantages. Newer high-definition digital cameras provide high quality video still images as well as high-resolution digital video, suitable for publication or teaching. Intrauterine Cutting and Hemostasis the instruments available for use through operative hysteroscopes include biopsy, grasping, cutting, and punch-biopsy devices. These tools are narrow and flexible enough to navigate the 1 to 2-mm diameter operating channel (Fig. Although their value is limited by their small size and flimsy construction; the scissors can divide adhesions, the biopsy forceps can sample targeted lesions, and the grasping forceps can remove small polyps or intrauterine devices. The uterine resectoscope is similar to the one used in urology and is designed to apply radiofrequency electrical energy in the endometrial cavity (Fig. An understanding of the principles of electrosurgery is mandatory for safe and effective use of this instrument. Tissue can be divided with a pointed electrode, excised with a loop, or desiccated with a rolling ball or bar. An electrode with multiple tips or edges can vaporize tissue, provided high generator outputs are used. A clear operative field is maintained by the continuous flow of nonconductive distending media in and out of the cavity. Although basic design modifications made the resectoscope more useful in gynecology, extraction of resected fragments is time consuming. The most effective approach is the periodic use of a uterine curette or polyp forceps inserted after removal of the hysteroscope. Manipulation of the electrode is via the white handle in the proximal portion of the device. Other Instrumentation For any hysteroscopic procedure, it is necessary to have available a cervical tenaculum, dilators, uterine curette, and appropriate-sized vaginal specula. When using the resectoscope, it is helpful to have a solid-state, isolated circuit electrosurgical generator capable of delivering both modulated and nonmodulated radiofrequency current. Laparoscopy or laparotomy may be necessary for emergencies secondary to uterine perforation. Other adverse events such as infection, excessive bleeding, and complications related to the distention media are extremely uncommon when the procedure is short and does not involve instrumentation of the myometrium (0% to 1%) (199). The risks of operative hysteroscopy are related to one of five aspects of the procedure performed: (i) anesthesia, (ii) the distention media, (iii) perforation, (iv) bleeding, and (v) thermal trauma (198,199). Anesthesia Local anesthetic protocols typically include the intracervical or paracervical injection of 0. Overdosage is prevented by ensuring that intravascular injection is avoided and by not exceeding the maximum recommended doses (lidocaine, 4 mg/kg; mepivacaine, 3 mg/kg). The use of a dilute vasoconstrictor such as epinephrine 1/200,000 reduces the amount of systemic absorption of the agent, virtually doubling the maximum dose that can be used and facilitates the onset of action of local anesthetic agents (220). Complications of intravascular injection or anesthetic overdose include allergy, neurologic effects, and impaired myocardial conduction. Allergy is characterized by the typical symptoms of agitation, palpitations, pruritus, coughing, shortness of breath, urticaria, bronchospasm, shock, and convulsions. Treatment measures include administration of oxygen, isotonic intravenous fluids, intramuscular or subcutaneous adrenaline, and intravenous prednisolone and aminophylline. Cardiac effects related to impaired myocardial conduction include bradycardia, cardiac arrest, shock, and convulsions. Emergency treatment measures include the administration of oxygen, intravenous atropine (0. The most common central nervous system manifestations are paresthesia of the tongue, drowsiness, tremor, and convulsions. The insufflator used must be especially designed for hysteroscopy; it is difficult to set laparoscopic insufflator flow rates below 1,000 mL per minute. Dextran 70 Dextran 70 is a hyperosmolar medium that, rarely, can induce an allergic response or coagulopathy (224,225). Similar to other types of distention media, if sufficient volumes are infused, vascular overload and heart failure can occur (226,227).
Buy seroquel 50 mg otc
An infusion of 50 fig of cosyntropin per hour was initiated 30 minutes before catheterization of the adrenal veins by the percutaneous femoral approach medicine abbreviations buy seroquel 100 mg low cost. Continuous infusion of cosyntropin is utilized in order to minimize stress-induced fluctuation in aldosterone levels, maximize the gradient in cortisol between the adrenal vein and the 699 inferior vena cava, and maximize the secretion of aldosterone from an adenoma. Venous samples were obtained from both adrenal veins (the left sided sample was obtained from the inferior phrenic vein near the entrance of the adrenal vein) and the inferior vena cava below the level of the renal veins. Concentrations of cortisol and aldosterone were measured in order to confirm correct catheter placement. Sampling was considered successful if the plasma level of cortisol in the adrenal vein was greater than five times that of the inferior vena cava. Aldosterone concentrations of each adrenal vein were divided by the respective cortisol concentrations to correct for an asymmetric dilutional effect between the adrenal veins. Using these criteria, a sensitivity of 95% and a specificity of 100% has been reported. In particular, this is due to difficulty in cannulating the right adrenal vein, the rate of which can be as low as 30% in low-volume centers. Our current approach to the evaluation of patients suspected of having primary aldosteronism is shown in Figure 16. Bilateral adrenal hyperplasia is usually best managed medically using the aldosterone antagonist spironolactone. Side effects of spironolactone, including gynecomastia, erectile dysfunction, menstrual disturbances, and muscle cramps can limit patient compliance. Most patients can achieve adequate control of their blood pressure with this medication alone or in conjunction with other antihypertensives. When an aldosterone-producing adenoma or unilateral adrenal hyperplasia is diagnosed, the appropriate treatment remains surgical resection. Unilateral adrenal hyperplasia cannot be differentiated from an adenoma preoperatively; nevertheless, the treatment is the same. Preoperatively, patients should be placed on spironolactone and given potassium supplementation to help normalize fluid and electrolyte balance over a 3 to 4-week period. Normalization of hypokalemia, aldosterone levels, and plasma aldosterone: renin ratio occurs in nearly 100% of patients with a unilateral aldosteronoma postoperatively. Up to 70% of patients will have resolution of hypertension after adrenalectomy, while 30% will require continued management with antihypertensive medications. Even those who require continued antihypertensive therapy will usually require fewer medications for adequate blood pressure control compared to preoperatively. Factors predictive of improvement or cure of hypertension after adrenalectomy include female gender, younger age, lower preoperative renin levels, shorter duration of hypertension (indicating that long-standing cardiovascular effects occur independent of aldosterone levels), and fewer antihypertensive medications preoperatively. Patients with primary aldosteronism have been shown to be at increased risk of cardiovascular and renal complications, including arrhythmias, myocardial infarction, stroke, chronic kidney disease, and death. Adrenalectomy decreases left ventricular diameter, volume, and workload, improves carotid artery stiffness, and reverses albuminuria. Adrenalectomy has also been shown to be more cost-effective than lifelong medical therapy in patients with primary aldosteronism amenable to surgical resection. Since nearly all patients with aldosteronomas have relatively small tumors which are universally benign, they are usually excellent candidates for a minimally invasive approach. Surgical resection can be performed either through a transabdominal laparoscopic or a retroperitoneoscopic approach. While the standard surgical approach for patients with an aldosteronoma is unilateral adrenalectomy, adrenal-sparing surgery (partial adrenalectomy) has been applied in selected patients with good results. Approximately 2% or less of adrenal cortical carcinomas cause isolated aldosteronism. In the very rare situation of a patient presenting with aldosteronism and a large adrenal mass, an open anterior approach should 702 be used to facilitate complete resection (see the section on adrenal cortical carcinoma). Cushing in 1932, and refers to a state of hypercortisolism that can result from a number of different pathologic processes (Table 16. Cortisol regulation involves feedback loops through the pituitary gland and hypothalamus. Carcinoma of the lung accounts for nearly three quarters of cases, with the remaining cases being caused by carcinoma of the pancreas, carcinoid tumors, medullary thyroid cancer, pheochromocytoma, and other neuroendocrine tumors. Ectopic secretion of corticotropin-releasing factor is exceedingly rare but has been reported in a few cases. The underlying cause is an adrenal adenoma 50% to 60% of the time and adrenal cortical carcinoma 20% to 25% of the time. Clinical Manifestations Weight gain is the most common feature of hypercortisolism and occurs predominantly in the truncal area. Abdominal striae, hypertension, hyperglycemia, depression, bruising, osteoporosis and menstrual irregularities can also occur. Children with Cushing syndrome have weight gain in association with decreased linear growth. Several studies have demonstrated that 2% to 3% of patients with poorly controlled diabetes mellitus have confirmed Cushing syndrome, while 5. Similarly, approximately 10% of patients with osteoporosis and a vertebral fracture were found to have Cushing syndrome. Adrenal cortical carcinomas can produce cortisol but often also produce androgens, resulting in virilization and hirsutism. Diagnosis Patients with Cushing syndrome have been shown to have an increased risk of cardiovascular and infectious complications, thus stressing the importance of early diagnosis and treatment. The evaluation for Cushing syndrome should be aimed at establishing the diagnosis first and then determining the etiology. Endocrine Society Clinical Practice Guidelines currently recommend first taking a thorough medication history, followed by testing of any patient with unusual features for age or multiple and progressive features (described above), in children with decreasing height and increasing weight, and in patients with an incidentally discovered adrenal mass. The secretion follows a diurnal variation: cortisol levels tend to be high early in the morning and low in the evening. The most sensitive initial screening test for hypercortisolism in patients with an adrenal mass is an overnight 1-mg dexamethasone suppression test (described below). Documentation of lack of cortisol suppression following 1 mg of dexamethasone should be followed by measurement of 24-hour urinary free (un-metabolized) cortisol; the normal level is generally below 80 fig/day. The most sensitive standard method for detecting hypercortisolism is the overnight one milligram dexamethasone suppression test. This test has a false negative rate of only 3% but unfortunately a false-positive rate of up to 30%. While a normal overnight dexamethasone suppression test excludes clinically significant hypercortisolism, an abnormal test result does not necessarily establish the presence of hypercortisolism but does require further investigation. Many experts currently propose further testing even in patients with serum cortisol values between 1. Naturally, when lower cutoffs are used, specificity decreases, yielding more false positives. The 24-hour urinary-free cortisol is somewhat less sensitive than overnight dexamethasone suppression but more specific. In patients who have obvious signs or symptoms of hypercortisolism, a timed urinary collection should be obtained for cortisol determination. It is recommended that patients submit at least two urine collections and the first morning void should be discarded. This test is not as accurate in patients with renal failure and those in the second and third trimesters of pregnancy. In equivocal cases, a formal 2-day low-dose dexamethasone test may be performed to detect the presence of cortisol overproduction by an adrenal tumor. Alternatively, individuals with failure of suppression after the 1-mg overnight dexamethasone test may be subjected to a higher dose (3 or 8 mg overnight suppression). Patients with true autonomous secretion of cortisol should continue to exhibit nonsuppression with these higher doses of dexamethasone. Treatment the appropriate management of Cushing syndrome depends on the underlying etiology. Patients with Cushing disease should undergo transsphenoidal hypophysectomy of the pituitary adenoma when it is believed to be resectable. Pituitary irradiation may also be used when resection is not curative, or otherwise judged not to be indicated.
Purchase seroquel 50 mg overnight delivery
Leak point pressure measurements often are performed at a bladder volume of 200 or 300 mL medicine ketoconazole cream purchase seroquel 200mg with mastercard. Patients are asked to cough with gradually increasing force (cough leak-point pressure) and finally to strain slowly (Valsalva) to increase intravesical pressure gradually. The lowest pressure at which leakage occurs is recorded as the cough or the Valsalva leak-point pressure (Fig. Many clinicians use a cutoff point of 60 cm water pressure to separate women who have intrinsic sphincter deficiency from those who do not. This is problematic for two reasons: (i) the marked variability of results that depend on all the aforementioned factors and (ii) the lack of prospective studies that demonstrate the predictive value of leak point pressure values on surgical outcomes. Medicare guidelines require that when bulking agents, such as collagen, are considered to treat stress incontinence, the intra-abdominal leak point pressure when the bladder has been filled with at least 150 mL of fluid must be less than 100 cm H O. Fluoroscopy and cystourethroscopy were used to visualize the bladder neck because many clinicians and investigators believe that a closed bladder neck is important in maintaining continence. However, studies of continent women reveal that many individuals with normal urethral function show evidence of bladder neck opening with physical stress (43). Neither test is recommended in the routine evaluation of women with straightforward incontinence. Voiding Cystometrogram Urodynamic testing usually concludes with an instrumented voiding study (also known as a pressure-flow study or voiding cystometrogram), in which the vesical, abdominal, and urethral pressures are measured simultaneously during bladder emptying (Fig. Various studies identified Valsalva voiding, low preoperative flow rate, and high preoperative detrusor pressures during voiding as risk factors for postoperative voiding dysfunction; however, findings often are contradictory. This patient voids in an uninterrupted flow pattern by means of a prolonged bladder contraction. She does not strain to void, with the exception of minimal straining toward the end of the flow. Imaging Tests the role of imaging techniques in studying female urinary incontinence is not yet established. Neurophysiologic Tests the neuromuscular function of the pelvic floor is dependent on the integrity of the nervous system. Pelvic floor neurophysiology utilizes techniques applied to nerves and skeletal muscles elsewhere in the body to document neuromuscular integrity or evidence of injury. These tests are not routinely used in the clinical evaluation of most incontinent women. Using a specialized electrode affixed over the index finger, the pudendal nerve is electrically stimulated near the ischial spine (either transrectally or transvaginally), and the resulting muscular response is measured. The latency time may be within the normal range when only smaller nerve fibers are affected; thus, neurologic dysfunction may exist in the presence of a normal latency time. Similar to the clinically obtained anal wink or bulbocavernosus reflex, electrically induced sacral reflexes can gather information about both the afferent and efferent arc in the pelvic nerves. A short train of dual impulses delivered next to the clitoris and measured at the anal sphincter is termed the clitoroanal reflex and provides information about the integrity of the afferent and efferent arm of the somatic pudendal nerve. A stimulating electrode placed in the bladder sends these signals along the visceral, autonomic fibers to the spinal cord, and a reflex signal will return along the pudendal nerve to the anal sphincter. Somatosensory Evoked Potentials Normal pelvic floor and pelvic organ function ultimately is controlled by higher centers in the central nervous system, including the cerebral cortex. Recording electrodes located on the scalp near the motor cortex allow the signal transmission speed between a skeletal muscle and the brain to be measured. Repeated electrical stimuli, called somatosensory evoked potentials, at a muscle of interest are used to assess the integrity of the central afferent limb. In a reverse fashion, electrical or magnetically induced stimuli can be delivered at the motor cortex (or along the spine), and the induced muscle action potentials can be detected. It is best used for simply describing the pattern and coordination of muscle activity but is less useful in providing more specific assessments. An increase in fiber density is evidence of previous nerve injury with successful reinnervation. Emerging Technologies Positron emission tomography and functional magnetic resonance imaging studies are yielding preliminary insights into the neural control of continence; these technologies are used in the research setting only. Nonsurgical Treatment Treatment of urinary incontinence can be either nonsurgical or surgical. The approach to treatment is based on the clinical findings and the degree of discomfort experienced by the patient, who should be fully informed of the risks and expected outcome. Lifestyle Changes Lifestyle interventions can decrease stress urinary incontinence in many women (45). There is good level 1 evidence that weight loss in both morbidly and moderately obese women decreases both stress and urge urinary incontinence (31). Postural changes (such as crossing the legs during periods of increased intra-abdominal pressure) often prevent stress urinary incontinence. There is some evidence that decreasing caffeine intake improves continence; however, fluid intake in general seems to play a minor role in the pathogenesis of incontinence. Although smokers are at greater risk for incontinence, no data were reported on whether smoking cessation resolves incontinence. Physical Therapy Medical evidence from well-designed randomized clinical trials shows that supervised pelvic floor muscle training (Kegel exercises) is an effective treatment for stress urinary incontinence. The Cochrane Incontinence Group concluded that pelvic floor muscle training is consistently better than no treatment or placebo treatment for stress incontinence and should be offered as first-line conservative management to women. Intensive training sessions that include personal contact with a health care professional to teach and supervise pelvic floor muscle training may be more beneficial than standard care. Biofeedback provides no added benefit over pelvic floor muscle training alone in women with stress urinary incontinence (46). Several factors improve the likelihood that pelvic muscle training will relieve stress urinary incontinence. The woman must do the exercises correctly, regularly, and for an adequate duration. Based on exercise training of skeletal muscles elsewhere in the body, many physical therapists recommend training sessions three to four times per week, with three repetitions of eight to ten sustained contractions each time. Electrical stimulation therapy was used to treat incontinence by delivering low levels of current via a probe placed in the vagina or rectum. Further research is needed to determine what niche this treatment may fill for women with urinary incontinence. Behavioral Therapy and Bladder Training Bladder training focuses on modifying bladder function by changing voiding habits. Behavioral therapy focuses on improving voluntary control rather than bladder function (51). She is instructed to empty her bladder when she awakes, and then every time during the day that the interval is reached (for example, every 30 to 60 minutes). When the patient feels the urge to void during that interval, she is instructed to use urge suppression strategies, such as distraction or relaxation techniques, until she gets to the stated interval. The main goal is to avoid running to the bathroom at the moment of severe urgency. Gradually, the interval is increased (usually weekly) until the patient voids every 2 to 3 hours. Bladder training is most effective when women record every void and check in (by telephone or in person) with a health care provider weekly. Bladder training is effective; in a trial in which bladder training was compared with treatment with oxybutynin, 73% of women in the bladder training group were clinically cured (52).
Order 200 mg seroquel overnight delivery
Relative contraindications to methotrexate therapy include gestational sac greater than or equal to 3 symptoms enlarged spleen purchase seroquel 300mg visa. Prior to the administration of methotrexate, a patient should have a complete blood count, blood type, liver function tests, electrolyte panel including creatinine, and a chest x-ray if there is any history of pulmonary disease. These studies are usually repeated 1 week after administration of methotrexate to evaluate for any potential complications from the therapy (190). Methotrexate Dosing Regimens Methotrexate is usually given via intramuscular injection but can be administered orally or by intravenous infusion. Methotrexate traditionally was administered using a multidose regimen, but single dosing protocols were developed that are easier for patient compliance (194). Patients receive 1 mg/kg of methotrexate intramuscularly on days 1, 3, 5, and 7 with leucovorin 0. If the methotrexate is discontinued early, the patient should receive leucovorin after her final dose of methotrexate to help reduce potential side effects. Earlier studies indicated approximately 19% will require all four doses, and 17% of women will require only one dose with this regimen (195,196). A more recent meta-analysis showed 10% of women require only one dose, while nearly 54% will require all four doses. Methotrexate Single-Dose Regimens Single-dose regimens were designed to increase patient compliance and simplify the administration of methotrexate. This regimen is well studied and safe and effective in the treatment of ectopic pregnancies. Compared with the multidose protocol, single-dose methotrexate is less expensive, patient acceptance is greater because less monitoring is required during treatment, and the treatment results and prospects for future fertility are comparable (194). Methotrexate Two-Dose Regimen the two-dose regimen was described as a cross between the single and multidose regimens. Because only 54% require all four doses of the multidose regimen, and 15% to 20% will require a second dose in the single-dose regimen, it is reasonable to consider a two-dose regimen of methotrexate. A single study showed an 87% success rate with low complication rates and high patient satisfaction (199). Effectiveness of Methotrexate the overall effectiveness of methotrexate therapy ranges from 78% to 96% (200). A meta-analysis in 2003 of 26 observational studies including 1,300 women revealed a significantly higher rate (93% versus. When comparing methotrexate to laparoscopic salpingostomy, the multidose regimen has similar success rates. After women receive additional doses as needed, the success rates are comparable between laparoscopic salpingostomy and single-dose methotrexate protocols (184). Signs of a tubal rupture include severe pain, hemodynamic instability, and a drop in hematocrit. Patients who report severe or prolonged pain should be evaluated by measuring hematocrit levels and performing transvaginal ultrasonography. The ultrasonography findings during follow-up, although usually not helpful, can be used to provide reassurance that the tube is not ruptured (203). Cul-de-sac fluid is a common finding, and the amount of fluid may increase if a tubal abortion occurs. It is not necessary to intervene surgically, unless the patient has a precipitous drop in hematocrit levels or she becomes hemodynamically unstable. Side Effects Side effects of methotrexate therapy are dose and frequency dependent. The most commonly reported side effects are the gastrointestinal symptoms of nausea, vomiting, stomatitis, and abdominal pain. Because of these potential effects, women are cautioned against using alcohol and nonsteroidal anti-inflammatory medications while being treated with methotrexate (190). Other side effects include bone marrow suppression, hemorrhagic enteritis, alopecia, dermatitis, elevated liver enzyme levels, and pneumonitis (204). These side effects are usually mild and self-limited; few life-threatening side effects are reported with methotrexate treatment for ectopic pregnancy. Long-term follow-up of women treated with methotrexate for gestational trophoblastic disease shows no increase in congenital malformations, spontaneous abortions, or tumors recurring after chemotherapy (205). Treatment of ectopic pregnancy differs from that of gestational trophoblastic disease in that a smaller total dose of methotrexate is required and shorter treatment duration is used. Although surgical management of ectopic pregnancy remains the mainstay of treatment worldwide, methotrexate treatment is appropriate in those patients who meet the treatment criteria previously detailed. Reproductive Outcome Reproductive function after methotrexate treatment can be assessed on the basis of repeat ectopic pregnancy rates, tubal patency, and pregnancy outcome. The risk of subsequent ectopic pregnancy is approximately 10% following either methotrexate or salpingostomy (52,53). The tubal patency rates are reported to be higher than 80% in those patients treated with either single-dose or multidose regimens with no difference in rates compared with women treated with salpingostomy (52,53). A randomized trial comparing methotrexate to laparoscopic salpingostomy showed no difference in tubal patency rates among the two groups, although in this trial patency rates were lower than previously reported at 66% in the salpingostomy group (206). Subsequent spontaneous intrauterine pregnancy rates are similar between those women treated with methotrexate versus salpingostomy, with rates ranging from 36% to 64% (207,208). Comparison of laparoscopically treated patients with methotrexate treated patients indicates that the two methods have similar reproductive outcomes. The potential advantages of salpingocentesis include a one-time injection with the potential avoidance of systemic side effects. Because of the limited experience, this treatment cannot be recommended until there is further study. This method has the obvious disadvantage of requiring laparoscopy, but it can be used if laparoscopy is performed for diagnosis. The proportion of ectopic pregnancies that resolve spontaneously and the reason they do so while others do not are unknown. There are no specific criteria for patient selection that predict successful outcome after spontaneous resolution. Persistent Trophoblastic Tissue Persistent ectopic pregnancy occurs when a patient underwent conservative surgery. Histologically, there is no identifiable embryo, the implantation usually is medial to the previous tubal incision, and residual chorionic villi are confined to the tubal muscularis. The incidence of persistent ectopic pregnancy increased with the increased use of surgery that conserves the tubes. Patients treated with laparoscopic salpingostomy have a higher rate of persistent ectopic pregnancies compared to those treated with salpingostomy at the time of a laparotomy, with an incidence of persistence after laparoscopic linear salpingostomy ranging from 4% to 15% (49,177). Persistent ectopic pregnancy can be treated surgically or medically; surgical therapy consists of either repeat salpingostomy or, more commonly, salpingectomy. Methotrexate offers an alternative to patients who are hemodynamically stable at the time of diagnosis. Chronic Ectopic Pregnancy Chronic ectopic pregnancy is a condition in which the pregnancy does not completely resorb during expectant management. The condition arises when there is persistence of the chorionic villi with bleeding into the tubal wall, which is distended slowly and does not rupture. It may arise from chronic bleeding from the fimbriated end of the fallopian tube with subsequent tamponade. In a series of 50 patients with a chronic ectopic pregnancy, pain was present in 86%, vaginal bleeding was present in 68%, and both symptoms were present in 58% (234). Ninety percent of the patients had amenorrhea ranging from 5 to 16 weeks (mean, 9.
Condamina (Carqueja). Seroquel.
- How does Carqueja work?
- Are there safety concerns?
- Are there any interactions with medications?
- Protecting the liver, diabetes, heart pain (angina), improving circulation, and other conditions.
- What is Carqueja?
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97071
Generic 200 mg seroquel fast delivery
There was an increase in hot 324 flushes symptoms xanax overdose purchase genuine seroquel on-line, fluid retention, and vaginal discharge associated with chemotherapy (Table 33). The study did not show any differential impact of tamoxifen for women with or without adverse pathological characteristics except for a nonsignificant indication that tamoxifen was less effective for women without comedo necrosis 6 or with smaller tumors. For that trial, three partial breast techniques are treated as equivalent: multicatheter brachytherapy, MammoSite balloon catheter, and 3-D conformational external beam radiation. This lack of differential effect suggests that treatment alone may not eliminate the adverse prognosis but also suggests that for patients with adverse prognostic features, treatment may be particularly important. Synthesizing across studies, we found no effects on overall mortality or breast cancer mortality (Table 35). All cancer events were reduced after combined treatment (lumpectomy plus radio and chemotherapy) when 324 compared to dual therapy (lumpectomy plus radiotherapy or lumpectomy plus 323,324 tamoxifen). A similar conclusion was reached with invasive breast cancer where mortality is much more common. Intent-to-treatanalyses: C ontroltreatment:L carcinoma orintracysticcarcinoma insitu,ongoingpregnancy, L ength offollowup(month s):100. A ssociationbetweentreatm entand patientoutcom es,stratified by arch itecture R elative M easure of N um berof M onth s of Treatm ent A uth or,Y ear Estim ate/Design A rch itecture th e A ssociation(95% W om en F ollowup C I) 357 L R vs. Lumpectomy+Radiation Fluid Retention 401 Lumpectomy+Radiation+ 1 study 1,781 74 1. Lumpectomy+Radiation Vaginal Discharge 401 Lumpectomy+Radiation+ 1 study 1,781 74 1. Lumpectomy or Lumpectomy+Tamoxifen Effects of Multiple Treatments Lumpectomy+Radiation+ Tamoxifen vs. Over this same period, incidence of invasive breast cancer has also increased dramatically from 105. The incidence of invasive breast cancer has also increased in all age categories, and the greatest increase has been in women over the age of 50. Comedo histology is associated with a particularly high risk of recurrence but has been more stable over recent years than noncomedo histology. The exact effect, however, is difficult to evaluate since they have not explicitly reported that there were no differences. Higher intake of soy foods was associated with a 406,407 modest, inconsistent decrease in breast cancer across studies. Moreover, limitations inherent in tissue processing make tumor measurement difficult. As a result, pathological examination can overestimate and underestimate tumor sizes depending on the plane of section. Estimates of the impact of these characteristics on survival shows a surprising lack of depth and, with few exceptions, is limited to studies of recurrence. When adjusting for demographic factors alone, African American women are more likely than white women to experience a recurrence. In some cases, these women have superior outcomes relative to white and African American women. The trial found that tamoxifen was associated with a 50 percent reduction in invasive ipsilateral and contralateral disease but had no impact on all-cause mortality. These trials would assess the potential benefit for the 26 percent of women whose tumors are positive for this adverse prognostic indicator. There are three accelerated radiation protocols, all of which reduce the time needed to complete therapy from 6fi weeks for whole breast radiation therapy to between 1 and 5 days. The treatment is focused on the area immediately around the lumpectomy site, the area where recurrences are most likely to occur. The arguments for a close relationship can be found in the similarity of risk factors for both the incidence of the diseases and their response to treatment. The following more detailed list of proposed recommendations (which expands on the table) are organized by the original questions: Question 1 1. Is it possible to use existing imaging technologies to distinguish between invasive and noninvasive cancer or between problematic and less problematic lesionsfi The answer has important implications for a discussion of the optimum post-diagnostic surveillance strategy. F uture research recom m endations Types ofStudies K ey Q uestion R esults ofL iterature R eview N eeded to A nswer F uture R esearch R ecom m endations Q uestion 1. C anbreastM R I predictinvasive canceraftercore sentinellymph node biopsy affect treatmentplanning needle biopsyfi Five-year outcomes of sentinel-lymph-node resection and results of a randomized clinical trial comparing total conventional axillary-lymph-node dissection in mastectomy and segmental mastectomy with or patients with clinically node-negative breast cancer: without radiation in the treatment of breast cancer. Noninvasive Comparison of Halsted mastectomy with breast carcinoma: results of a national survey by the quadrantectomy, axillary dissection, and radiotherapy American College of Surgeons. Ten-year trends in breast cancer among younger women in the results of a randomized trial comparing a United States. J Natl Cancer Inst 2008 Nov 19; conservative treatment to mastectomy in early breast 100(22):1643-8. Trends in situ of the breast in the population-based the treatment of ductal carcinoma in situ of the surveillance, epidemiology and end results program. Overdiagnosis Cochrane handbook for systematic reviews of and overtreatment of breast cancer: estimates of interventions. J Comparative effectiveenss of core needle and open Clin Oncol 2007 May 20; 25(15):2127-32. Treatment of early-stage grading the quality of evidence and the strength of breast cancer. N Engl J grading the quality of evidence and the strength of Med 1981 Jul 2; 305(1):6-11. University of California-San Francisco-Stanford the experience of the Institut Gustave-Roussy. Statistics in pathology of breast cancer detected by mass Medicine 1999; 18(24):3435-51. Clinical analysis of observational studies in epidemiology: a efficacy of mammographic screening in the elderly. The use of numbers needed to treat cancer in the Detroit metropolitan area (1975-1988). Int J Cancer 1996 May Cochrane handbook for systematic reviews of 16; 66(4):413-9. Publication bias in meta-analysis: the relative incidence of impalpable invasive breast its causes and consequences. J Clin Epidemiol 2000 carcinoma and ductal carcinoma in situ in cancers Feb; 53(2):207-16. Collaborative Group of carcinoma in situ of the breast, a population-based Readers of the Breast Cancer Screening Program of study of epidemiology and pathology. Nation-wide breast cancer screening in the rates of advanced breast cancer due to Netherlands: results of initial and subsequent mammography screening in the Netherlands. Mammogram a screening program by age: should older women screening of Chinese women in Kwong Wah continue screeningfi A comparison incidence patterns among in situ and invasive breast of screening mammography results from programs carcinomas,with possible etiologic implications. Cancer Epidemiol Biomarkers Prev Cancer Epidemiol Biomarkers Prev 2000 Jul; 2005 Apr; 14(4):1008-11. Interval cancers as an indicator breast cancer: incidence trend and organised of performance in breast screening. Ann Intern Med 2000 Dec 5; cancer: a prospective multicentre cohort study 133(11):855-63. J Gen Intern Med 2001 Nov; 16(11):779 biopsy outcome after mammography: what is the 84. J Natl Cancer of changing from one to two views at incident Inst 2002 Oct 16; 94(20):1546-54. Recent trends and programme in England: impact on cancer detection racial/ethnic differences in the incidence and and recall rates. Cancer 2003 Feb 15; 97(4):1099 aided detection with screening mammography in a 106. J Rural Health 2003 Differences in screening mammography outcomes Fall; 19(4):470-6.

Order seroquel 200 mg on line
Although not specifically studied schedule 8 medications list discount seroquel master card, the incidence of hysterectomy for fibroids declines considerably after menopause, suggesting that there is a significant decline in symptoms. A placebo-controlled, double-blind study of 25 women with menorrhagia, 11 of whom also had fibroids, found a 36% decrease in blood loss among women with idiopathic menorrhagia, but no decrease in women with fibroids. Reduction in uterine size occurs mostly within the first 3 months of treatment (88). Seventy-eight percent experience hot flushes, 32% vaginal dryness, and 55% have transient frontal headaches. Arthralgia, myalgia, insomnia, edema, emotional lability, depression, and decreased libido are reported. Although not specifically studied, add-back therapy might be considered in this setting. A prospective, randomized, controlled trial of mifepristone treatment found a 48% decrease in mean uterine volume after 6 months (95). Mifepristone blocks progesterone, and the unopposed exposure of the endometrium to estrogen may lead to endometrial hyperplasia. A systematic review found endometrial hyperplasia in 10 of 36 (28%) women screened with endometrial biopsies (96). Twenty-two of 26 (85%) women with documented fibroid-related menorrhagia returned to normal bleeding within 3 months. By 12 months, 27 of 67 (40%) women had amenorrhea and 66 women had hemoglobin levels above 12 g/dL. After 12 months, mean estimated blood loss, measured by pictorial blood loss assessment, decreased from 392 to 37 mL with an associated increase in hemoglobin levels. Alternative Medicine Treatment A nonrandomized, nonblinded study compared fibroid growth in 37 women treated with Chinese medicine, body therapy, and guided imagery to 37 controls treated with nonsteroidal anti-inflammatory medications, progestins, or oral contraceptive pills (100). After 6 months, sonographic evaluation demonstrated that fibroids stopped growing or shrank in 22 of 37 (59%) women treated with Chinese medicine compared to 3 of 37 (8%) controls. Although symptoms responded equally well in both groups, satisfaction was higher in the Chinese medicine group. Participants actively sought alternative therapy, however, and assessment of satisfaction may reflect selection bias. An uncontrolled study reported treatment of 110 women with fibroids smaller than 10 cm with the Chinese herbal medicine kuei-chih-fu-ling-wan for at least 12 weeks (101). Clinical and sonographic evaluation found complete resolution of fibroids in 19% of women, a decrease in size in 43%, no change in 34%, and an increase in 4%. Menorrhagia improved in 60 of 63 (95%) of women and dysmenorrhea improved in 48 of 51 (94%). Fifteen of the 110 (14%) women chose to have a hysterectomy during the 4 years of the study. Surgical Treatment Options Surgical treatment options currently include abdominal myomectomy, laparoscopic myomectomy, hysteroscopic myomectomy, endometrial ablation, and abdominal, vaginal, or laparoscopic hysterectomy. Serious medical conditions, such as severe anemia or ureteral obstruction, often need to be addressed surgically. Pain from fibroid degeneration is usually successfully treated with analgesics until symptoms resolve, but if severe the patient may opt for surgery. Torsion of a pedunculated subserosal fibroid may produce acute pain that requires surgical intervention. Surgical intervention may be indicated in women with fibroids associated with menorrhagia, pelvic pain or pressure, urinary frequency, or incontinence that compromises quality of life (102). Abdominal myomectomy was long employed as a conservative treatment for uterine fibroids, and much of the literature predates the use of prospective, randomized controlled trials. A prospective, nonrandomized study comparing myomectomy with uterine artery embolization did report that 75% of women in the myomectomy group had a significant decrease in symptom scores after 6 months (105). Back pain may, on occasion, be related to the presence of fibroids, but other possible causes should be considered. Inability to evaluate the ovaries on pelvic examination is not an indication for surgery (106). There is no evidence that pelvic examination increases early detection or decreases the mortality related to ovarian cancer, and sonography can be used to evaluate the adnexa should symptoms develop. Treating Preoperative Anemia Recombinant Erythropoietin Severe anemia can be rapidly corrected using recombinant forms of erythropoietin and iron supplementation. Erythropoietin alfa and epoetin are commonly used to increase preoperative hemoglobin concentrations in cardiac, orthopaedic, and neurologic surgery. A prospective, nonrandomized study of epoetin given preoperatively found a significant increase in hemoglobin concentrations prior to , and following, gynecologic surgery (108). Abdominal Myomectomy Myomectomy should be considered a safe alternative to hysterectomy. A retrospective review of 197 women who had myomectomies and 197 women who underwent hysterectomies with similar uterine size (14 versus 15 weeks) found operating times were longer in the myomectomy group (200 versus 175 minutes), but estimated blood loss was greater in the hysterectomy group (227 versus 484 mL) (111). The risks of hemorrhage, febrile morbidity, unintended surgical procedure, life-threatening events, and rehospitalization were no different between groups. However, 26 (13%) women in the hysterectomy group suffered complications, including 1 bladder injury, 1 ureteral injury, 3 bowel injuries, 8 women with ileus, and 6 women with pelvic abscesses. In contrast, complications occurred in 11 (5%) of the myomectomy patients, including 1 bladder injury, 2 women with reoperation for small bowel obstruction, and 6 women with ileus. Myomectomy may be considered even for those women who have large uterine fibroids and wish to retain their uterus. The cell saver, which is a devise used to collect blood intraoperatively and reinfuse, was used in 70 women, and only 7 required homologous blood transfusion. A retrospective cohort study compared 89 women having abdominal hysterectomy for fibroids (mean uterine size 15 cm) to abdominal myomectomy in 103 women (mean uterine size 12 cm) (113). Although selection bias was likely, the hysterectomy group suffered two ureteral, one bladder, one bowel, and one nerve injury and two reoperations for bowel obstruction, while there were no visceral injuries in the myomectomy group. Cesarean Section and Concurrent Myomectomy In carefully selected women, myomectomy may be safely accomplished at the time of cesarean section by experienced surgeons. One series reported 25 women with removal of 84 fibroids (2 to 10 cm) at the time of cesarean section without the need for cesarean hysterectomy (114). Estimated blood loss was 876 mL (range 400 to 1,700 mL) and five women required blood transfusion. Another study compared 111 women who had myomectomy at the time of cesarean section with 257 women with fibroids who were not subjected to myomectomy during cesarean section (115). Only one of the women in the myomectomy group required transfusion and none required hysterectomy or embolization. There were no differences in mean operative times, incidence of fever, or length of hospital stay between the two groups. Although the cases were likely selected carefully, the authors concluded that, in experienced hands, myomectomy might be safely performed in selected women during cesarean section. Surgical Technique for Abdominal Myomectomy Managing Blood Loss Available surgical techniques allow safe removal of even large fibroids. Vasopressin, an antidiuretic hormone, causes constriction of smooth muscle in the walls of capillaries, small arterioles and venules. Rare cases of bradycardia and cardiovascular collapse were reported; intravascular injection should be carefully avoided and patients should be carefully monitored (118). The use of vasopressin to decrease blood loss during myomectomy is an off-label use of this drug. Use of the cell saver avoids the risks of infection and transfusion reaction, the oxygen transport capacity of salvaged red blood cells is equal to or better than stored allogeneic red cells, and the survival of red blood cells appears to be at least as good as transfused allogeneic red cells (119). The device suctions blood from the operative field, mixes it with heparinized saline, and stores the blood in a canister. If the patient requires blood reinfusion, the stored blood is washed with saline, filtered, centrifuged to a hematocrit of approximately 50%, and given back to the patient intravenously. Consequently, the need for preoperative autologous blood donation or heterologous blood transfusion often can be avoided (120).

Cheap seroquel online master card
A ctive treatment:L R L ength offollowup(month s):102 Exclusioncriteria:Pagetdisease ofnipple treatment for chlamydia buy 300 mg seroquel amex,priororconcurrentinvasive or C ontroltreatment:N one. Design:C ase-series L ength offollowup(month s):51 Exclusioncriteria:M icroscopicaxillary L N involvement,priororconcurrentinvasive A ctive treatment:M A ge:M edian50. Design:C ase-series N umber:367 Exclusioncriteria:A priororsynch ronous infiltratingductalcarcinoma. Design:C ase-series N umber:109 Exclusioncriteria:W omenwith microinvasionorreceivingth eirtreatmentand A ctive treatment:L R L ength offollowup(month s): followupelsewh ere. L ength offollowup(month s):47 Strategyto reduce bias:Stratification A ge:M ean56 (19-82) Variables:M argin,tumorsiz e,necrosis,nucleargrade,and treatment. A ctive treatment:M,L,L R L ength offollowup(month s):91 Strategyto reduce bias:Stratificationand multivariate adjustment C ontroltreatment:N one. R egistry Design:case-series L ength offollowup(month s):N A Exclusioncriteria:N one. R egistry C ountry:N eth erlands C entre Eastinth e N eth erlands Exclusioncriteria:Patients with a h istory ofora simultaneous invasive breast (retrospecti Design:C ase-series N umber:798 cancerand oth ermalignancies (exceptfornonmelanoma skincancerand insitu ve analysis A ctive treatment:M,M R, L ength offollowup(month s):59 cervicalcarcinoma),ormedicalrecords notavailable forreview. Outcomes: Combined ipsiliateral unknown/missing radiotherapy status or surgery status. Registry Design: case-series Number: 1,036 Exclusion criteria: Women treated by mastectomy or lumpectomy and radiation (retrospecti Active treatment: L Length of followup (months): 77. Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es C ontroltreatment:N one. Design:C ase-series N umber:230 Strategyto reduce bias:Stratification A ctive treatment:L R L ength offollowup(month s):98. Design:C ase-series N umber:126 Strategyto reduce bias:Stratification A ctive treatment:L R orL L ength offollowup(month s):N A Variables:Excisionvolume and radiationinstratification. A ctive treatment:L R N umber:132 Exclusioncriteria:C ases with invasive ormicroinvasive carcinoma ofth e breast, C ontroltreatment:N one L ength offollowup(month s):84 initialdetectionbyanymeth od oth erth anmammograph y,orincomplete path ologic A ge:N A (20% <45 years) review. A ctive treatment:L R N umber:146 Exclusioncriteria:C ases with microinvasive cancers orpriorcontralateralinvasive C ontroltreatment:N one L ength offollowup(month s):85. A ctive treatment:L,L R, N umber:237 Strategyto reduce bias:multivariate analysis Table F 26. Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es L T,orL R T L ength offollowup(month s):47 Variables:M argin,grade,and tumorsiz e inmultivariate analysis. Design:case-series M ich igan Exclusioncriteria:C ases with invasive ormicroinvasive carcinoma ofth e breast,or A ctive treatment:L R N umber:148 incomplete path ologicreview. R egistry Design:C ase-series L ength offollowup(month s): Exclusioncriteria:C ases with no followuptime,errors incause-of-death codes, (retrospecti A ctive treatment:N A wh ite:<50,96;50-59,92. Poormammogram quality,orwith outimagingth e cancer;combined ipsiliateral entire area ofth e breast. Design:C ase-series M ich igan Exclusioncriteria:Invasive ormicroinvasive carcinoma orincomplete path ologic A ctive treatment:L R N umber:148 review. Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es Design:C ase-series N umber:124 Strategyto reduce bias:Stratificationand multivariate analysis A ctive treatment:M L ength offollowup(month s):60 Variables:N otspecified inmultivariate analysis. Design:C ase-series N umber:705 Exclusioncriteria:Patients underwentmastectomy A ctive treatment:L R L ength offollowup(month s):84 Strategyto reduce bias:Stratificationand multivariate adjustment C ontroltreatment:L A ge:M ean53. Design:C ase-series N umber:660 Strategyto reduce bias:Stratification A ctive treatment:L R L ength offollowup(month s):88 Variables:M argininstratification. A ctive treatment:L L ength offollowup(month s):57 Strategyto reduce bias:Stratificationand multivariate adjustment C ontroltreatment:N one A ge:N A Variables:M argin,age,nucleargrade,tumorsiz e,and necrosis inmultivariate O utcomes:C ombined ipsiliateral analysis. Design:case-series N umber:227 Strategyto reduce bias:Stratification A ctive treatment:M,L R, L ength offollowup(month s):56 Variables:A rch itecture instratification. A ctive treatment:M orL R L ength offollowup(month s):51 Strategyto reduce bias:Stratification C ontroltreatment:N one A ge:M ean52 (27-82) Variables:A rch itecture instratification. A ctive treatment:L R L ength offollowup(month s):81 Strategyto reduce bias:N one. Design:C ase-series N umber:310 Strategyto reduce bias:Stratification A ctive treatment:L R orL L ength offollowup(month s): Variables:A ge,race,family h istory,margin,tumorsiz e,nucleargrade,necrosis, C ontroltreatment:N one 103. A ctive treatment:L R N umber:177 Exclusioncriteria:C ases with invasive ormicroinvasive carcinoma ofth e breast, C ontroltreatment:L L ength offollowup(month s):84 initialdetectionbyanymeth od oth erth anmammograph y,orincomplete path ologic A ge:N A (18% <45) review. A ctive treatment:L R N umber:132 Exclusioncriteria:C ases with invasive ormicroinvasive carcinoma ofth e breast, C ontroltreatment:N one L ength offollowup(month s):84 initialdetectionbyanymeth od oth erth anmammograph y,orincomplete path ologic A ge:M edian56 (31-84) review. F rauenklinik der Strategyto reduce bias:N one A ctive treatment:M,L R, U niversitatM unch en Variables:N one orL N umber:161 C ontroltreatment:N one L ength offollowup(month s):78. A ctive treatment:L R L ength offollowup(month s): Exclusioncriteria:Pagetdisease ofnipple,priororconcurrentinvasive or Table F 26. Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es C ontroltreatment:N one 111. Design:C ase-series U K Strategyto reduce bias:Stratificationand multivariate analysis A ctive treatment:M,L R, N umber:220 Variables:Distance from nipple to lesion,nucleargrade,and radiationth erapy in L T,L R T,orL L ength offollowup(month s):132 multivariate analysis. Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es A ge:M ean60. Design:C ase-series oranoth erh ospitalinM ich igan Exclusioncriteria:C ases with invasive ormicroinvasive carcinoma ofth e breast,or A ctive treatment:L R N umber:513 incomplete path ologicreview. G roup2:a minimum clearmargin Design:C ase-series N umber:153 10mm orreexcisionmarginclear,tumorsiz e <16mm,low to intermediate nuclear A ctive treatment:L R L ength offollowup(month s):99 grade,and notreceive R T. C ontroltreatment:L A ge:median55 (N A) Exclusioncriteria:R eceivingmastectomy(112),goingelsewh ere fortreatment(4), O utcomes:C ombined ipsiliateral and positive marginrefusingreexcisiom(4). Sum m ary ofch aracteristics ofincluded observationalstudies (continued) Source and N um berof Patients,F ollowupDuration L evelof Study K ey Inclusion/ExclusionC riteria,Strategy to R educe B ias,Variables (m onth s),A ge (R ange),and Evidence O utcom es A ctive treatment:L orL R L ength offollowup(month s):57. Total all mortality Number of Rate (or Probability) of Author Followup Duration Participants Events All cause mortality 251 Jhingran, 2002 150 120 0. Total all mortality (continued) Number of Rate (or Probability) of Author Followup Duration Participants Events 294 96 0. Total breast cancer mortality Number of Rate (or Probability) of Author Followup Duration Participants Events Breast cancer mortality 251 Jhingran, 2002 150 120 0 171 Kestin, 2000 132 120 0. Total breast cancer mortality (continued) Number of Rate (or Probability) of Author Followup Duration Participants Events 162 Silverstein, 2003 280 81 0. Total distant metastasis Number of Rate (or Probability) of Author Followup Duration Participants Events Distant Metastasis 246 Kricker, 2004 945 51. Total regional recurrence Number of Followup Rate (or Probability) of Author Participants Duration Events Regional Recurrence 160 Cutuli, 2001 716 91 0. Total local invasive Number of Followup Rate (or Probability) of Author Participants Duration Events Local Invasive Recurrence 238 Habel, 1998 709 120 0. Total local invasive (continued) Number of Followup Rate (or Probability) of Author Participants Duration Events 188 Cutuli, 2002 515 84 0. Total local invasive (continued) Number of Followup Rate (or Probability) of Author Participants Duration Events 254 Roka, 2004 132 61. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) M am m ograph icdensity/contralateralinvasive carcinom a 185 H wang,2007 L orL R H igh vs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) fi5mm from margin,tumorsiz e,nucleargrade,necrosis, meth od ofdetection,and excisionvolume 174 Vicini,2000 L R C lose/involved vs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) 188 C utuli,2002 L Positive/unknownvs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) adjusted by detection method, margin, nuclear grade, Total sample size: 1,036 and type of calcification 1-1. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) recurrence,adjusted by margin,age,grade,tumorsiz e, Totalsample siz e:445 and necrosis 238 H abel,1998 L R orL fi15mm vs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) 237 O mlin,2006 L R orL 2 vs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) 232 Idvall,2003 L 3 vs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) meth od ofdetection,and re-excisionvolume 10637243 L R <40mlvs. O bservationalstudies ofth e associationbetweencontroland system aticoutcom es and tum orch aracteristics (continued) R elative R isk or F ollowupDurationand A uth or,Study Design,and A djusters Treatm ents Predictor H az ard R atio TotalSam ple Siz e (95% C I) 160 C utuli,2001 L R fi60 vs.
Cheap 100 mg seroquel otc
Or medicine man dr dre order generic seroquel online, insert them Close the wound loosely, leaving a corrugated drain below the inner eyebrows. An infected joint is another condition in which failure to drain pus early is a real disaster: severe chronic and 7. If you do not drain the infected joint early, it will be destroyed and may ultimately ankylose. In a child, the epiphyses near it may the spine can rarely be affected by suppurative osteitis: displace, or dislocate. As soon as you have made the the patient is usually a very ill child with fever and severe diagnosis, drainage is urgent: this is not an operation to back pain, usually in the lumbar region. If you allow pus to accumulate some inflammatory oedema over the spine, which is very under pressure in the hip, it may impair the blood supply tender, and may be arched backwards by muscle spasm, as to the head of the femur within 8hrs, so that it necroses. There may be paraplegia as the result of inflammatory Bacteria can reach a joint: oedema involving the cord. Before the age of 6 months from osteomyelitis in the survival the pus must be drained by removing the metaphyses of any long bone. After this age the epiphyseal transverse processes of some of the vertebrae and part of plates prevent spread like this. At any age in the hip, because the proximal metaphysis probably occur in 3-6 months. But if there are extensor, or of the femur is partly within the capsule of the hip joint. There is the hip may also be infected in a child as a result of pain, but little or no fever, and no arching of the back. Through the blood from a distant septic focus, spondylodiscitis (infection of the disc space). Ambulatory treatment arthritis, which involves the knee, hip, shoulder, and ankle with standard anti-tubercular therapy is effective if patients in this order of frequency. Through a penetrating wound of a joint, especially of when neurological signs ensue. Drainage is required if there is no joints, commonly the hip or knee, becomes so painful that response to antibiotics, neurological signs ensue, or there moving it even a little in any direction causes great pain. Later, if the infected joint is near the surface, you will be If the bodies of the vertebrae are abnormal, but not the able to feel that it is warm and swollen with fluid. Unfortunately, the shoulder and the hip are so deep that If the disc and the adjoining bone are diseased, you cannot easily detect fluid, so that the only local sign is especially if this is maximal anteriorly, suspect infection. In the very old or very young, there may be few Osteitis of the pubis may occasionally follow general signs of infection, and the effusion may not even symphysiotomy (21. You can easily confuse tuberculous with subacute Congenital syphilis presents as swelling of both knees suppurative arthritis. Review the progress at 3 & 6wks, when suppurative arthritis should Several things can happen to a severely damaged joint: show much improvement, whereas it is still too early for (1) It can dislocate. She was given physiotherapy, nursed on a fracture bed for 3wks, and discharged on crutches. Some weeks later she was readmitted, pyrexial, and with a swelling of her right thigh extending from her knee to her iliac crest. This was settling nicely when she developed pain in her left hip and became pyrexial. The radiographs of her hip were normal, septic arthritis was diagnosed, and she was given large doses of the latest broad-spectrum antibiotic. Two years later her pain was so severe that she had to have her hip disarticulated. At best she will have a painful hip, either for life, or until her hip has ankylosed spontaneously, or been fused surgically. Frank pus in the syringe, or even slightly cloudy synovial the diagnosis is particularly difficult in babies: fluid, confirms the diagnosis. This in itself was unusual, because, enough; it only tells you that pus is present: you must if a baby does this, he usually draws up both of them. He was found to have suppurative arthritis of the right hip, which was too painful to move. Septic arthritis is more common in the disadvantaged and If you fail to aspirate a joint that you think is infected, malnourished and also in infancy and old age. Culture the synovial fluid (30% +ve most frequent organism in newborns, but is seldom seen in result) and blood (14%). You may see the first signs of new bone formation as early as the 5th day in an infant, but it will not appear before the 10th day in an older child, and may take longer. Try to isolate the organism, otherwise cloxacillin or chloramphenicol are most suitable. If, when you drain an infected joint and wash out the pus, its joint surfaces are smooth, there is a good chance of having a normal or nearly normal joint. The prognosis is worse if cartilage has been lost, if the joint surfaces are rough, if the bone is soft, or if the radiograph shows severe joint destruction. Use a tourniquet where possible, and if the hand is involved, watch out for its nerves. The linear incision you have just made will become elliptical, and you will see the cartilage underneath. If the joint surfaces feel rough but some cartilage still covers the bones, there may still be useful function in the joint. G kindly contributed by Jack if it is done too early, there will be growth problems so delay this as long as possible. The position of function is the best position for a joint to be in if it is going to be fixed, or if its movement is going 7. It is also called the position for (except the hip) ankylosis Joints need to be in particular positions for particular the position of rest is the most comfortable position for a purposes, so be sure to get it right. Put it into this position if it has to be rested for coincide with one another, and the position of function is any reason, but is in no danger of ankylosing. Keeping the Any kind of ankylosis, stable or unstable, is a dreadful needle horizontal, push it 30fi medially into the joint space, disability if the joint becomes fixed in the wrong position, from a point just under the postero-inferior border of the so make sure that, if it is going to ankylose, it does so in acromion (7-15G). The position of function varies Anterior route: this is easier but more hazardous. You never know for sure when a joint space between the pectoralis major and deltoid muscle. Slope it laterally 30fi and knee just short of full extension; splint the right push it backwards, until it enters the loose pouch under the (or dominant) elbow flexed. Do not leave this task to a physiotherapist in the hope that it will be achieved later! Put the shoulder into a spica in 45fi of abduction, with the elbow just anterior to the coronal plane, in 70fi of medial rotation so that the hand can reach the mouth. Feel for the head of the radius, the olecranon and the lateral epicondyle of the humerus. Using these points of a triangle, push the needle through its centre into the posterolateral aspect of the joint. Stay close to the olecranon, and remember that the posterior interosseous nerve winds round the neck of the radius 3cm distal to its head. A, notice that the shoulder is abducted, the right elbow is Keep the arm in a sling in 90fi of flexion. For example, Muslims and many other With the knee extended, make a 5cm incision 2cm behind peoples write and eat with their right hands and use their the medial edge of the patella and its tendon. If so, the right elbow should the quadriceps expansion, longitudinally, and put a curved be more flexed than the left. The dominant elbow will haemostat into the suprapatellar pouch, under the surface probably be most useful if it is flexed 10fi beyond a right of the patella. Put your finger into the joint and use it to angle, with the forearm pronated 45fi so that feeding, remove the pus. Dress the wound and apply skin traction, If both the elbows are going to ankylose, arrange their or a plaster backslab. Without one or other a painful positions so that the dominant arm can reach the mouth.

