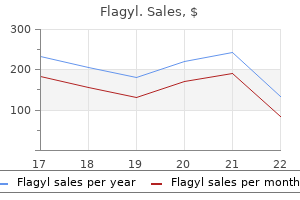
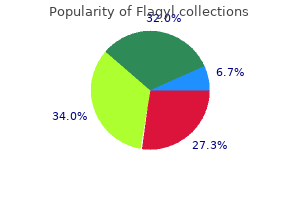
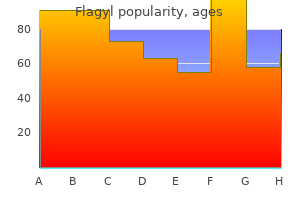
Flagyl
Purchase 500mg flagyl overnight delivery
Although the incidence of infection is high virus 5ths disease buy flagyl 400mg line, most infections resolve spontaneously. A small proportion of infected persons become persistently infected; persistent infection is the most important risk factor for the development of cervical cancer. However, laboratory reagents used for these assays are not standardized and there are no standards for setting a threshold for a positive result. Medical management depends on treatment of the specific clinical manifestation of the infection (such as genital warts or abnormal cervical cell cytology). Transmission occurs most frequently with fi Temporal pattern sexual intercourse but can occur following nonpenetrative None sexual activity. In a prospective study of college women, the cumulative incidence of infection was 40% by 24 months after first sexual intercourse. Communicability can be presumed to be high because of the large number of new infections estimated to occur each year. Results of epidemiologic studies are less consistent for other risk factors, including young age at sexual initiation, number of pregnancies, genetic factors, smoking, and lack of circumcision of male partner. Population-based estimates, primarily from clinics treating persons with sexually transmitted infections, indicate that about 1% of the sexually active adolescent and adult population in the United States have clinically apparent genital warts. This exceeds the economic burden of any other sexually transmitted infection except human immunodeficiency virus. Cervical Cancer Screening Most cases and deaths from cervical cancer can be Cervical Cancer Screening prevented through detection of precancerous changes within the cervix by cervical cytology using the Pap test. Currently fi Revised in 2012 available Pap test screening can be done by a conventional fi Screening should begin at age Pap or a liquid-based cytology. Since 2012, all organizations have recommended that screening should begin at age 21 years. While there are slight differences in other aspects of the recommendations, all groups recommend screening in women aged 21 to 65 years with cytology (Pap test) every 3 years. It is available in 2 types fi a 9-valent vaccine licensed in of prefilled syringes. However, there is no known serologic contains types 16 and 18 correlate of immunity and no known minimal titer (high risk) determined to be protective. The high efficacy found in the clinical trials to date has precluded identification of a minimum protective antibody titer. Further follow-up of vaccinated cohorts may allow determination of serologic correlates of immunity in the future. Study populations will continue to be type did not diminish efficacy followed for any evidence of waning immunity. Males aged 22 through 26 years without age these risk factors may be vaccinated as well. The second and third doses should be administered 1 to 2 and 6 months after the first dose. The third dose need not be repeated as long as it was administered at least 16 weeks after the first dose and at least 12 weeks after the second dose. If the series is interrupted after the first 6 months dose, the second dose should be given as soon as possible, fi An accelerated schedule using and the second and third doses should be separated by an minimum intervals is not interval of at least 12 weeks. If only the third dose is delayed, recommended it should be administered as soon as possible. Administering all indicated vaccines at a single visit increases the likelihood that adolescents and young adults will receive each of the vaccines on schedule. Each vaccine should be administered using a separate syringe at a different anatomic site. However, the immune response and vaccine efficacy might be less than that in persons who are immunocompetent. A moderate or severe acute illness a vaccine component or is a precaution to vaccination, and vaccination should be following a prior dose deferred until symptoms of the acute illness improve. The vaccine has not been causally associated with adverse pregnancy outcomes or with adverse effects on the developing fetus, but data on vaccination during pregnancy are limited. However, if a woman is found to be pregnant after initiation of the vaccination series, the remainder of the series should be delayed until after completion of the 183 Human Papillomavirus pregnancy. In prelicensure clinical trials, local reactions, such fi Women vaccinated during as pain, redness or swelling were reported by 20% to 90% pregnancy may be reported to of recipients. However, fi Local reactions (pain, redness, reports of fever did not increase significantly with increasing swelling) doses. However, these symptoms occurred with equal associated with either vaccine frequency among both vaccine and placebo recipients. Manufacturer package inserts contain additional information and can be found at. Lauri Markowitz and Elizabeth Unger for their assistance in updating this chapter. United States Cancer Statistics; 1999-2009 Incidence and Mortality Web-based Report. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2013. Genital human papillomavirus infection incidence and risk factors in a cohort of female university students. Some types may cause wart-like bumps to form on the penis, in and around the vagina, and on the cervix and anus. Warts may appear as wart-like growths or may be flat and only slightly raised from the skin. People that have had unprotected sex with more than two partners in their life have probably already been exposed to the wart virus. For most people warts are only a bother, and are treated only for cosmetic reasons. There are several different chemicals (treatments) that can be used to remove the warts. Some of these are available for home use; ask your clinician if these are right for you. Talk to your clinician if you have been told you have wart virus on the cervix there are special treatments available for this. You may also want to talk to your clinician about evaluation and experimental treatments that are now being offered in some settings for anal warts. Warts may return, even after treatment because the virus stays in the skin once you are infected. If your warts are not gone after your treatment today, you may return every 3 weeks for more treatment overuntil they are gone. People that have had unprotected sex with more than two sex partners in their life have probably already been exposed to the wart virus. Having genital warts or a partner with warts does not necessarily mean you need to get a Pap Test. For more information: Please talk with your City Clinic clinician or your own health care provider. The age, gender, education and marital status, age of first sexual intercourse, Turkey number of sexual partners, sexual orientation, and smoking status were recorded in both groups. No significant differences were found based on sexual orientation or condoms between the patient and control groups. In the patient group, the mean age of first sexual intercourse was significantly earlier, and the number of single individuals and sexual partners were significantly higher. Also, 61% of the patients were current smokers, which was significantly higher than the control group. Early age of first sexual intercourse, a high number of sexual partners, being single, and smoking were also risk factors for the development of anogenital warts.
Best 250mg flagyl
Reasoning first articulated at the dawn of modern sex-equality doctrine continues to supply authority for the diferential treatment of mothers and fathers the infection 0 origins movie buy 500mg flagyl with amex. The failure to see gender diferentiation in parenthood as a sex-equality problem led law to devalue the social contributions of unmarried biological fathers. In the contemporary regulation of par2347 the yale law journal 126:2260 2017 entage, this failure also leads law to discount the social contributions of women who separate parenthood from biological ties. The Court has focused on questions of classification and discriminatory purpose in ways that mask inequality. Courts might conclude that so long as the government treats nonbiological unmarried parents the same (closing paths to their parental recognition), it acts in accordance with principles of equal protection. Certainly, these doctrinal features complicate efective constitutional oversight in the law of parental recognition. Yet, critically, these features did not prove dispositive in judicial approaches to marriage equality. Instead, courts considered social meaning in ways that led them to repudiate forms of exclu438 sion that had long been taken for granted. Scholars have pointed out how Obergefell may authorize discrimination against nonmarital family bonds. Of course, there are strong arguments that laws prohibiting same-sex marriage classify on the basis of sexual orientation. Sexual-Orientation Equality and Parental Recognition the approach to equality that guided resolution of the marriage question could shape approaches to questions of parental recognition. Disputes emerging in state courts under state constitutional law are illustrative. For the court, the efect of the law on same-sex couples appeared more important than a formal approach to questions of classification. The concern with social meaning in marriage equality jurisprudence extends to parent-child relationships. Hodges, which noted that the right to marry provides benefits not only for same-sex 453 couples, but also the children being raised by those couples. Nonrecognition and resort to adoption are concrete harms infiicted on same-sex parents and their children. Siegel, the American Civil Rights Tradition: Anticlassification or Antisubordinationfi Sex Equality and Parental Recognition While the constitutional treatment of gays and lesbians has evolved dramatically in recent years, the law of sex equality has received less attention. Yet issues of gender diferentiation in parenthood continue to arise in both family law and immigration law. Constitutional precedents have permitted this system by citing biological diferences between women and men to authorize the diferential treatment of mothers and fathers. In Nguyen, the Court upheld regulations making it more difcult for fathers to confer citizenship on nonmarital children. They treat sex-based classifications as presumptively unconstitutional and subject such classifications to heightened scrutiny regardless of whether they implicate physiological 463 diferences between women and men. They recognize that in some circumstances, sex-based classifications can be justified in light of physiological difer464 ences. The tension between Virginia and Nguyen manifests itself most clearly in the law of parental recognition. If courts were to reason about parenthood from Virginia, rather than Nguyen, they would likely exhibit less tolerance for gender diferentiation. This term, the Court has before it another case challenging the diferential 465 treatment of unmarried mothers and fathers in the immigration context. The law imposed longer residency requirements on unmarried fathers who wished to transmit citizenship to their children. In 2011, an equally divided Court 466 afrmed per curiam a Ninth Circuit decision upholding these regulations. As Reva Siegel shows, even when the Court reasons in what many consider to be an anticlassification framework, it ofen vindicates antisubordination values. In rejecting the regulations now before the Court, the Second Circuit re468 fused to extend Nguyen. Indeed, the father had legitimated the child by marrying the 471 mother when the child was eight. Decisions on questions of parenthood in immigration may shape decisions in family law, just as earlier decisions relating to family law underwrote subsequent decisions regarding citizenship status. State court reasoning that relies on Nguyen to justify the nonrecognition of nonbiological mothers for purposes of parentage law could become suspect. The biological father and his wife had been raising the child, who at the time of the deci467. See Siegel, supra note 122, at 264-65 (discussing how questions of gender equality are obscured by physiological reasoning about reproduction in the legal regulation of abortion).
Discount flagyl 400mg visa
Traditional surrogacy requires no medical intervention and is usually arranged informally between the 13 parties concerned bacterial 16s rrna universal primers discount flagyl 250mg amex. Any resulting child would be regarded as the child 17 of the commissioning parents and raised by them. The oocytes and/or sperm used to create the embryo(s) can be either from the commissioning parents or from a donor(s) and there is no genetic relationship between the surrogate and the child. Thus, several adults may be involved in the creation of a child through gestational surrogacy, including one or two commissioning parents, one or two donors, and the surrogate mother. The International Federation of Fertility Societies cites the following as indications for surrogacy: (1) Patients without a uterus, but with one or both ovaries functioning; (a) Women with congenital absence of the uterus; (b) Women who have had a hysterectomy for carcinoma or other reasons; (2) Women who suffer repeated miscarriage and for whom the prospect of carrying a baby to term is very remote. In the United Kingdom, the Human Fertilisation and Embryology Authority advised clinics that surrogacy should be considered only when it was physically impossible or highly undesirable for medical reasons for the commissioning mother to carry a pregnancy, but lifted these restrictions in its revised Code of Practice published in 2009 at. In Australia, the responsibility for regulating surrogacy is vested in the States and Territories. Although State and Territory governments agreed to harmonise surrogacy legislation throughout 29 Australia, there is currently variation between the legislation of each jurisdiction. In addition to adhering to State and Territory legislation, fertility clinics are obliged to abide by country-wide ethical 30 guidelines and a professional accreditation scheme. The legal and regulatory restrictions applied to surrogacy in Australia mean that it is not accessible to some individuals or couples for whom it might otherwise be a viable family-building option. The greatest hurdle for undertaking surrogacy in Australia is finding a woman who is willing 35 and able to be a surrogate without being financially compensated. Furthermore, in South Australia 36 and Western Australia gay men are explicitly excluded from access to surrogacy. For those who are unable to find a surrogate, overseas commercial surrogacy provides a potential opportunity to have a child. Transfer of parentage following surrogacy Until November 2000 no Australian State or Territory provided for the transfer of parentage from the 37 surrogate to the commissioning parents when a child was born as the result of surrogacy. Since State and Territory laws vest parentage of a child in the birth mother (in common with many other jurisdictions), the surrogate is regarded as the legal mother regardless of her genetic relationship to the 38 child. Commissioning parents who wished to formalise their parental relationship with a child born following surrogacy were compelled to do so by applying for a residence or parental responsibility 39 40 41 order under the Family Law Act 1975 (Cth). In Victoria and New South Wales, commissioning parents could also apply to adopt the child in very restricted circumstances where the surrogate and commissioning parents were members of the same family. The momentum for State and Territory law to provide specifically for the transfer of parentage following a surrogacy arrangement built as a result of: media interest in, and the apparent increasing 31National Health and Medical Research Council, n 30 at [13. Possession of an order enables commissioning parents to make educational and medical decisions for the child and allows for the issue of a passport, but does not grant parental status and expires once the child reaches 18 years of age. In 2000, the Australian Capital Territory became the first Australian jurisdiction to address the 46 legal status of the child born following surrogacy. The 2004 Act removed discrimination related to parentage with the recognition of same-sex partners and introduced a new requirement that neither the surrogate (birth mother) nor her partner may be the genetic parent of the child. Children born overseas to a non-Australian surrogate are not regarded as the legal children of the Australian commissioning parents under State or Territory law, or generally under federal law, regardless of genetic links to one or both, or the recognition of them as the parents in a foreign birth 53 certificate or court order. An application for parental responsibility can be made if the commissioning parents are Australian. However, practically, the commissioning parents need to bring the child into Australia prior to consideration of an application in the Family Court of Australia. The Family Law Act 1975 (Cth) interacts with State and Territory surrogacy legislation in relation to parentage. In the resulting 2009 proposals, the Committee stated: [t]he proposed model would not permit commercial surrogacy. It is judged that commercial surrogacy commodifies the child and the surrogate mother, and risks the exploitation of poor families for the benefit of rich ones. In practice, State and Territory laws and regulations relating to surrogacy are still not harmonised and significant differences between them remain (Table 1). Most notable is the criminalisation of extraterritorial commercial surrogacy in some jurisdictions. Turkey is the only other jurisdiction in 62 the world where undertaking extraterritorial surrogacy is a criminal act. The motivation behind this measure was to avoid the commodification of children and surrogates and economic exploitation of vulnerable women, particularly in developing countries where surrogacy is a proliferating business and protective regulation is absent. The Hon Linda Burney, who was responsible for introducing the measure in New South Wales, argued in parliamentary debate that: [b]y making commercial surrogacy an extraterritorial offence we will help to prevent exporting this exploitation of women overseas. In some countries where commercial surrogacy is allowed, such as the United States, some regulation is in place to protect the wellbeing of surrogate mothers. In my mind it would be irresponsible and indeed immoral to legislate in New South Wales but to be silent on the potential exploitation by our own citizens of vulnerable women overseas. In laissez-faire fertility markets overseas, poor women have no protection they give up the right to be able to change their mind after birth. For example, the Hon David Shoebridge argued: the urge to have a family is overwhelming for many people. Many people driven by an overwhelming urge to have a child will travel to jurisdictions in which commercial surrogacy is not illegal States in America have sophisticated laws that deal with commercial surrogacy arrangements. Making entering into those arrangements unlawful in New South Wales will not stop couples from heading off to those jurisdictions. In fact, it will only make criminals of those people for entering into an arrangement that they will enter into in any event. First, early judgments have cast doubt on the willingness of either the judiciary or law enforcement agencies to take exemplary action against Australians who disregard the ban on undertaking commercial surrogacy overseas. In two recent cases involving applications for parental responsibility following declared commercial surrogacy, the Family Court judge referred his judgments to the Office of the Director of 66 Public Prosecutions to consider whether the commissioning parents should be prosecuted. The applicants in one of these cases had entered into surrogacy arrangements with two surrogates. While their first application for parental responsibility was referred to the Office of the Director of Public Prosecutions, their second application was heard by a judge who awarded them parental responsibility without any such referral. To date, no prosecutions for breach of the extraterritorial surrogacy laws had been instituted by government law agencies. Secondly, some Australian couples who have contravened extraterritorial surrogacy legislation are taking evasive action to avoid drawing attention to themselves. A survey conducted by Surrogacy Australia and recent media reports have revealed that some commissioning parents are eschewing parentage order applications or relocating to jurisdictions where extraterritorial commercial 68 surrogacy is not explicitly banned.
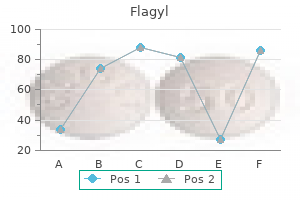
| Comparative prices of Flagyl | ||
| # | Retailer | Average price |
| 1 | Ace Hardware | 949 |
| 2 | ShopKo Stores | 748 |
| 3 | Amazon.com | 700 |
| 4 | Whole Foods Markets | 773 |
| 5 | Family Dollar | 984 |
| 6 | Advance Auto Parts | 215 |
| 7 | Office Depot | 332 |
| 8 | Best Buy | 542 |
Buy 500 mg flagyl with mastercard
The consensus was that there is currently insufficient evidence to recommend the use of antenatal breast milk expression in women with gestational diabetes outside the clinical trial setting antibiotics buy purchase generic flagyl line. The Guideline Development Team recognises that information on lifestyle (diet, exercise and appropriate weight gain) is important throughout the pregnancy and into the postpartum period. The specificity was fixed at 100%, as all the oral glucose tolerance tests with negative results will necessarily have a fasting blood glucose < 7. Screening, diagnosis and management of gestational diabetes in New Zealand: 43 A clinical practice guideline 9. The HbA1c test (alone or in combination with fasting glucose test) lacked diagnostic test accuracy in detecting abnormal carbohydrate metabolism in women who have had gestational diabetes at a mean follow-up of 13 months postpartum (Picon et al 2012). The lack of postpartum screening has also been associated with the test not being requested by the physician (Dietz et al 2008). Five times as many women returned for postpartum screening when both they and their physician received a reminder. The proportion of women undergoing postpartum screening was lower than in the randomised trial (28% versus 60%) but the reminder system doubled the screening rate (14% usual care, 28% with reminder) (Shea et al 2011). Laboratory forms were misplaced and women often did not have access to child care at the time of the test. A follow-up study on 110 women in Northland treated for gestational diabetes found almost onethird (32%) had abnormal glucose results at follow-up (mean 2. Uptake of postpartum screening was very low (30%) and the diagnosis of diabetes in half of the women was as a direct result of the study. Of those with abnormal results, 66% were Maori and 95% of those diagnosed with diabetes had required insulin during pregnancy (McGrath et al 2007). The use of HbA1c may miss a number of women with lower levels of hyperglycaemia, but will detect women with the highest glucose levels who will require immediate assessment. HbA1c is currently used to screen for diabetes in New Zealand in the non-pregnant population. The progression of HbA1c over time is an important concept that is not captured by cross-sectional studies. The initial test is a one-step method that is likely to engage the woman and her general practitioner in the process of regular follow-up testing and review of healthy lifestyle interventions (+/metformin). When women are planning another pregnancy, the HbA1c is a useful way of identifying which women are at increased risk of miscarriage or congenital anomaly, because of elevated glucose levels, and who may benefit from pre-pregnancy counselling. Women should be informed through a variety of media about the importance of postpartum screening for diabetes following gestational diabetes. The reasons for non-adherence to postpartum screening in New Zealand may need further exploration. Screening, diagnosis and management of gestational diabetes in New Zealand: 47 A clinical practice guideline Chapter 10: Type 2 diabetes in women diagnosed with gestational diabetes 10. Identification of potentially modifiable risk factors that are indicative of significantly increased risk of developing type 2 diabetes may be useful in targeting prevention strategies. The risk of recurrence of gestational diabetes in subsequent pregnancies ranges between 30% and 84% following the index pregnancy (75% for women who were treated with insulin). One of the strongest predictors of type 2 diabetes postpartum was elevated intrapartum fasting plasma glucose levels. Lean women (under 30 years of age) who received insulin therapy during pregnancy were more likely to develop type 1 diabetes postpartum (Canadian Diabetes Association 2008). The percentage of women with impaired fasting glucose or impaired glucose tolerance ranged from 2. There is variation in diagnostic criteria, the populations included and the percentage of women that returned for postpartum screening. The incidence of impaired fasting glucose or impaired glucose tolerance ranged from 15% (in a migrant population) (Girgis et al 2012) to 48. Data are not pooled in a meta-analysis due to the high likelihood of heterogeneity from different populations and diagnostic thresholds. There is growing evidence to suggest that the risk of developing type 2 diabetes is increased for women with an abnormal screening glucose but normal oral glucose tolerance test (p < 0. The evidence identified a number of key risk factors for developing type 2 diabetes in women diagnosed with gestational diabetes. Continued intensive surveillance of women with a history of gestational diabetes is important for early detection and treatment of diabetes. A lack of long-term follow-up in women with gestational diabetes may mean that a high proportion of women have undiagnosed diabetes. Other risk factors contributing to development of type 2 diabetes in women with gestational diabetes are: fi pre-pregnancy overweight or obesity fi high diagnostic glucose levels fi high glucose levels during pregnancy fi early gestational age at diagnosis of gestational diabetes fi elevated postpartum oral glucose tolerance test. Screening, diagnosis and management of gestational diabetes in New Zealand: 51 A clinical practice guideline Chapter 11: Prevention of type 2 diabetes in women diagnosed with gestational diabetes 11. The Diabetes Prevention Program randomised participants to either standard lifestyle and placebo, or metformin (an oral hypoglycaemic) or an intensive lifestyle intervention (Ratner et al 2008; refer to Appendix P, Table 48). The authors estimate that only five to six women would need to be treated over three years with either metformin or intensive lifestyle intervention to prevent one case of diabetes. In women without a history of gestational diabetes, the estimated numbers needed to treat to prevent a single case of diabetes over three years are 24 for metformin and 9 for intensive lifestyle intervention (Ratner et al 2008). Women with a history of gestational diabetes were less able to sustain the prescribed level of physical activity, resulting in a significantly lower weight loss over time than women without a history of gestational diabetes. There is a reduction of over 50% in the risk of type 2 diabetes following structured lifestyle interventions in the high-risk groups (refer to Appendix P, Table 49; for details of the goals in the included trials, refer to Appendix P, Table 50). No statistically significant effects on diabetes incidence were observed when comparing exercise-only interventions either with standard recommendations or with diet-only interventions (Orozco et al 2008). A small, multicentre, pilot randomised controlled trial from Australia compared telephone-based motivational interviewing with standard care in 28 rural-based women with previous gestational diabetes. The intervention group significantly reduced total fat intake, total carbohydrate intake and glycaemic load. They increased leisure physical activity, although there was no significant change in total physical activity levels, and significantly reduced their body mass index compared with the control group (Reinhardt et al 2012). A second pilot trial examined a postpartum lifestyle intervention adapted from the Diabetes Prevention Program (Ferrara et al 2011). The intervention significantly decreased dietary fat intake more than the usual care (p = 0. A one-year (interim) report on the feasibility of a lifestyle intervention programme found no significant differences in changes in fasting glucose and two-hour glucose after an oral glucose tolerance test. Key point fi Lifestyle interventions may be useful in preventing type 2 diabetes in women who have had gestational diabetes but they require motivation from the individual and are resource intense. Thiazolidinediones significantly reduced the relative risk of diabetes by 50% compared with biguanides and trended towards a 40% risk reduction compared with alpha-glucosidase inhibitors (Phung et al 2011). A Cochrane systematic review of oral anti-diabetic agents for women with pre-existing diabetes mellitus/impaired glucose tolerance or previous gestational diabetes failed to identify any suitable trials, highlighting a large gap in the research available to guide clinical practice (Tieu et al 2010a). Key point fi Metformin may be a useful treatment in women who have had gestational diabetes and who continue to have impaired glucose tolerance despite lifestyle interventions, especially if they are planning another pregnancy. The Guideline Development Team agreed that the primary focus for preventing type 2 diabetes needs to be on lifestyle interventions and acknowledged the potential role of green prescriptions in women with high risk of developing diabetes. The decision to fund a screening programme or treatment uses scarce resources which have competing uses. The review included one French study that recommended high-risk screening and an Italian study that found universal screening was more costly than the selective screening approach per case of gestational diabetes diagnosed. No incremental analysis was reported and the review authors concluded that screening using either strategy was justified. A strategy of universal oral glucose tolerance test was predicted to detect an additional 1493 cases compared with the universal fasting plasma glucose, at a cost per additional case detected of fi4,665. Four studies reported the estimated cost per case of gestational diabetes detected.
Buy cheap flagyl on-line
Gestational Carrier nd further agrees that after the start of the 32 week of gestation in a singleton pregnancy antibiotic 500 mg purchase flagyl 400 mg mastercard, or after the th start of the 28 week of gestation in a multiple pregnancy, she will remain within 100 miles of the hospital where she is expected to deliver and will not travel to the State of Washington. Gestational Carrier agrees that she will continue to reside within the State of Oregon from the time this Agreement is signed until after the completion of any resulting pregnancy. Gestational Carrier specifically agrees to undergo an induction and/or a cesarean section if her obstetrician advises her to do so for a medical reason. Gestational Carrier agrees to undergo blood tests and ultrasounds to evaluate hormonal levels throughout the term of this Agreement. Gestational Carrier shall undergo in vitro fertilization/embryo transfer, during which embryos will be transferred to Gestational Carrier. If Gestational Carrier does not become pregnant after the first embryo transfer procedure, the Parties intend to attempt up to two (2) more embryo transfer procedures during subsequent cycles that Intended Parents agree to complete within eight (8) months after the date of the first embryo transfer procedure. The Parties intend that only one embryo will be transferred to Gestational Carrier in any given cycle, but may mutually agree to transfer a different number at a later date. Gestational Carrier understands that she may be required to stay on bedrest, may not be able to perform her regular activities, and may be prohibited from traveling for a period of time after the embryo transfer procedure. If, at any time, Gestational Carrier is found to be incapable of carrying a child, neither Intended Parents nor Gestational Carrier shall be under any further obligation with respect to this Agreement and this Agreement shall terminate. However, any expenses, including but not limited to medical and legal expenses, incurred pursuant to this Agreement through the date of termination of this Agreement shall remain the obligation of Intended Parents. If the pregnancy is terminated by miscarriage or otherwise in accordance with this Agreement, Gestational Carrier is entitled to receive a prorated portion of the $30,000. Such compensation is due regardless of whether the child is diagnosed to have a terminal condition or is born with substantial medical abnormalities. If the child does not survive birth by seven (7) days, Gestational Carrier is entitled to receive a prorated portion of the $30,000. Except as otherwise provided in this Agreement, Gestational Carrier is entitled to receive and retain the entire base compensation if she delivers a child after completing 32 weeks of pregnancy, regardless of whether the child is viable, stillborn, dies shortly after birth, is released from the hospital, is diagnosed to have a terminal condition, or is born with substantial defects or abnormalities. Any prorated compensation paid pursuant to this Agreement shall be calculated based on the conventional 40 week gestational calendar. This means that Gestational Carrier will be considered to be more than two (2) weeks pregnant at the time of the embryo transfer. If Gestational Carrier is pregnant with multiples, the base compensation will be increased by $5,000. These payments will begin upon ultrasound confirmation of a multiple pregnancy and continue for each month during which Gestational Carrier remains pregnant with multiples. If at any point it is determined that Gestational Carrier is no longer pregnant with multiples, she will retain the monthly payments she has already received, but will not receive any further distribution of the multiples fee. If the embryo transfer is unsuccessful, Gestational Carrier shall receive the same sums if she undergoes subsequent cycles. Cancelled Cycle If the cycle is cancelled due to no fault of Gestational Carrier and she has begun taking injections, she will keep the $500. Maternity Clothing If a pregnancy is confirmed, Gestational Carrier will receive $500. In other words, Gestational Carrier will receive the payment after she begins medical screening appointments or after all parties have signed the Agreement, and she is waiting to begin a cycle, waiting between cycles, or is pregnant. If Gestational Carrier and Intended Parents agree that Gestational Carrier will provide breast milk for the Child after birth, then the monthly expense allowance will continue for so long as the provision of breast milk continues. Gestational Carrier is not required to provide receipts for expenses paid pursuant to this section. Cesarean Section If Gestational Carrier delivers by cesarean section for medical reasons, she shall receive $1,500. Invasive Procedures If Gestational Carrier undergoes a required invasive procedure related to a pregnancy achieved pursuant to this Agreement, including but not limited to amniocentesis, chorionic villi sampling, biopsy, selective reduction of pregnancy or D&C, she shall receive $750. If Gestational Carrier undergoes a termination of pregnancy pursuant to the terms of this Agreement that is performed after the end of the thirteenth week of gestation, she shall receive $2,000. Loss of Uterus, Fallopian Tubes, or Ovaries If Gestational Carrier suffers a loss of her uterus as a result of the performance of her obligations under this Agreement, she shall receive $5,000. Additionally, if Gestational Carrier suffers a loss of one or more fallopian tubes or ovaries as a result of the performance of her obligations under this Agreement, she shall receive $2,500. Intended Parents shall not be responsible for any compensation under this section if the loss occurs more than three months after the date of delivery, termination or miscarriage. Life Insurance Intended Parents agree to pay for a term life insurance policy for Gestational Carrier that provides coverage in the amount of $350,000. Intended Parents are responsible for paying the premiums and shall maintain the life insurance for eight weeks after the date of birth. The funds provided by Intended Parents for surrogacy-related counseling will be available for a maximum of one year following birth and are available only for the purpose of counseling. It is the responsibility of any person receiving payments or reimbursements pursuant to this Agreement to determine the tax consequences and to make any necessary reports to the federal and state taxing authorities. Gestational Carrier has provided Intended Parents with a copy of her policy and proof of coverage so that Intended Parents can review the policy before they incur or pay any expenses pursuant to this Agreement. Intended Parents have had an opportunity to review the policy and they are satisfied with the coverage. If Intended Parents ask Gestational Carrier to obtain a different or supplemental health insurance policy, Intended Parents will pay the premiums for the new policy for coverage beginning when the insurance is obtained and continuing for eight (8) weeks after delivery, termination of pregnancy, miscarriage or a failed embryo transfer, unless there are ongoing complications from the pregnancy or birth at eight (8) weeks, in which case they will continue to be responsible for the premiums for a maximum of eight (8) additional weeks. Gestational Carrier agrees to cooperate in applying for any such alternate insurance. Gestational Carrier agrees to use her medical insurance for the medical procedures contemplated by this Agreement. These notices include, but are not limited to , cancellation notices, past payment due notices, changes in coverage, or denial of coverage. The Parties shall make their own investigation of the existence and extent of coverage for the conduct contemplated by this Agreement.
Buy flagyl 200mg with mastercard
However antibiotic spectrum order cheapest flagyl, there are still some adults born prior to 1957 that have had neither the vaccine nor the disease and thus remain susceptible. If a student in your school develops confirmed measles, your local health officer may require implementation of the following control measures: a. Outbreak control measures listed above also apply to all staff at the affected school. Diagnosis is made by a spinal tap and a blood or joint culture, depending on the symptoms. Report to your local health jurisdiction immediately suspected or confirmed cases of meningitis or outbreaks associated with a school. Referral to licensed health care provider of suspected cases is immediate and mandatory for meningitis. Exclude from school until licensed health care provider releases student in consultation with your local health jurisdiction. Teachers and the parent/guardian should contact their licensed health care provider or local health jurisdiction if they have further questions about preventive measures. Your local health jurisdiction will provided specific guidance in these situations. Instruct students not to share items that may be contaminated with saliva such as beverage containers. The meningococcal conjugate vaccines can be used at ages as early as 9 months for certain high risk infants/toddlers. Cover any wound that is draining or has pus with a clean, dry bandage that is closed on all four sides. If a draining wound cannot be safely covered, consult with health care provider to determine when it is safe for a student to return. Strongly encourage showering with soap immediately after participating in sports involving close personal contact. Having atopic dermatitis, the most common type of eczema, also increases the risk of getting Molluscum Contagiosum. In healthy individuals, these lesions ultimately disappear without scarring, unless there is excessive scratching, which may leave marks. Because Molluscum Contagiosum is self-limited in healthy individuals, treatment may be unnecessary. Participation in close-contact sports such as wrestling and basketball, or those that use shared equipment like gymnastics and baseball should be avoided unless all lesions can be covered by clothing or bandages. Seek guidance from the licensed health care provider to determine when the student can safely return to these activities. Other items and equipment (such as kick boards and water toys) should be used only when all bumps are covered by clothing or watertight bandages. In some cases, covering the lesions with a bandage may help stop scratching and spread of the virus. Around 80 percent of people infected with West Nile virus will not show any symptoms. Encephalitis is an inflammation of the brain with severe symptoms including high fever, headache, neck stiffness, disorientation, convulsions, muscle weakness, vision loss, numbness, paralysis, and coma. Over 30,000 cases of West Nile virus infection have been reported in this country with 45 cases acquired in Washington State. Mosquitoes become infected with the West Nile virus when they feed on infected birds, particularly crows and related birds. Encourage field trip participants to wear a long sleeved shirt, long pants, and a hat when going into mosquito-infested areas such as wetlands or woods. Mumps patients may have fever, headache, and mild respiratory symptoms or may have no symptoms other than parotitis. Mode of Transmission Transmission is by direct contact with or droplet spread of the saliva of infected persons. It should be remembered that approximately one-third of all susceptible individuals exposed to mumps will not develop apparent disease but will still be infectious. Infectious Period Mumps virus has been found in the saliva from 7 days before to 9 days after the onset of parotitis (salivary gland infection). However, persons with mumps are most contagious from 2 days before the onset of illness to 4 days after swelling first appears. Noroviruses are highly contagious and as few as 10 viral particles may be sufficient for infection. Immediately report to your local health jurisdiction suspected or confirmed foodborne outbreaks associated with a school. The local health jurisdiction may issue additional requirements for food handlers. Antibacterials such as triclosan and general use disinfectants such as quarternary ammonium compounds are not generally effective against norovirus and related viruses. Therefore, due to the different types of noroviruses, individuals are likely to be repeatedly infected throughout their lifetimes. Most foodborne outbreaks of norovirus are likely to arise through direct contamination of food by a handler immediately before its consumption. Outbreaks have frequently been associated with cold foods, including salads, sandwiches, and bakery products. Liquid items, such as salad dressing or cake icing that allow the virus to mix evenly, are often implicated in outbreaks. Waterborne outbreaks of norovirus in community settings have often been caused by sewage contamination of wells and recreational water. Despite these features, it is likely that relatively simple measures such as correct handling of cold foods, no barehand contact with ready-to-eat food by foodworkers, and frequent hand washing, may substantially reduce foodborne transmission of noroviruses. Children under the age of 1 year are much more liable to suffer serious consequences than older children. Communicability gradually declines and is negligible by 3 weeks after the onset of paroxysms. Make referral to licensed health care provider of suspected case for diagnosis and treatment. Your local health officer will make recommendations regarding treatment of school and household contacts. Although some infected individuals have no symptoms, pinworm infestation can include severe anal itching with disturbed sleep, restlessness, and local irritation from scratching. Response to specific antihelminth drugs (drugs that kill parasitic worms) is excellent, but re-infestation occurs easily. The initial symptoms may include fever, tiredness, gastrointestinal upset, headache, and sore throat. Although wild polio transmission has ceased in most countries as a result of vaccination programs, it remains endemic in a few areas of the world, and importation remains a threat. Mode of Transmission Transmission of the virus can occur by contact with pharyngeal (throat) droplets as well as through fecal-oral spread. Polio is most infectious in the few days before and after the onset of clinical symptoms. Internationally, polio control is achieved by immunization of any individual in an epidemic area who is over the age of 6 weeks and who is unvaccinated, incompletely vaccinated, or uncertain of vaccination history. Instruct students not to share combs, hats, towels, and/or other personal articles. Future Prevention and Education Ringworm of the body is not particularly dangerous, has no unusual long-term consequences, and can generally be treated quite effectively with locally applied preparations. Instruct students about the causes, means of transmission, and prevention of this condition. The rash usually consists of pink to red isolated spots that appear first on the face then spread rapidly to the trunk, biceps, and thigh areas of the extremities with large confluent areas of flushing.
Cheap flagyl 200mg without prescription
Intrapartum Management Optimal timing of delivery relies on balancing the risk of intrauterine fetal death with the risks of preterm birth antibiotic resistance of bacterial biofilms buy generic flagyl from india. Early delivery may be indicated in some patients with vasculopathy, nephropathy, poor glucose control, or a prior stillbirth. In contrast, patients with well-controlled diabetes may be allowed to progress to their expected date of delivery as long as antenatal testing remains reassuring. Expectant management beyond the estimated due date generally is not recommended. To prevent traumatic birth injury, cesarean delivery may be considered if the estimated fetal weight is greater than 4,500 g in women with diabetes. Induction of labor in pregnancies with a fetus with suspected macrosomia has not been found to reduce birth trauma and may increase the cesarean delivery rate. During induction of labor, maternal glycemia can be controlled with an intravenous infusion of regular insulin titrated to maintain hourly readings of blood glucose levels less than 110 mg/dL. Avoiding intrapartum maternal hyperglycemia may prevent fetal hyperglycemia and reduce the likelihood of subsequent neonatal hypoglycemia. Patients who are using an insulin pump may continue their basal infusion during labor. One half of the predelivery dose may be reinstituted after starting regular food intake. Breastfeeding should be encouraged in women with pregestational diabetes mellitus. Thyroid Disease Because thyroid disease is the second most common endocrine disease that affects women of reproductive age, obstetricians often care for patients in whom alterations in thyroid gland function have been previously diagnosed. In addition, both hyperthyroidism and hypothyroidism may initially manifest during pregnancy. During pregnancy, the diagnosis of thyroid abnormalities is confused by significant but reversible changes in maternal thyroid physiology that lead to alterations in thyroid function tests during gestation. However, there are gestational age-specific nomograms and thresholds for evaluating thyroid status during pregnancy. The presence of maternal thyroid disease is important information for the pediatrician to have at the time of delivery. Thyroid Function Testing Thyroid testing in pregnancy should be performed on symptomatic women and women with a personal history of thyroid disease or other medical conditions associated with thyroid disease (eg, type 1 diabetes mellitus). The performance of thyroid function tests in asymptomatic pregnant women who have a mildly enlarged thyroid is not warranted. Development of a significant goiter or distinct nodules should be evaluated as in any patient. Women with established overt thyroid disease (hyperthyroidism or hypothyroidism) should be appropriately treated to maintain a euthyroid state throughout pregnancy and during the postpartum period. The signs and symptoms of hyperthyroidism include nervousness, tremors, tachycardia, frequent stools, excessive sweating, heat intolerance, weight loss, goiter, insomnia, palpitations, and hypertension. Thyroid storm is a serious complication of inadequately treated Graves disease that can adversely affect both mother and fetus. Late distinctive symptoms of Graves disease are Obstetric and Medical Complications 223 ophthalmopathy (signs including lid lag and lid retraction) and dermopathy (signs include localized or pretibial myxedema). Compared with controlled maternal hyperthyroidism, inadequately treated maternal hyperthyroidism is associated with a greater risk of preterm delivery, severe preeclampsia, and heart failure and with an increase in medically indicated preterm deliveries, low birth weight infants, and possibly fetal loss. Hyperthyroidism in pregnancy is treated with thioamides, which decrease thyroid hormone synthesis by blocking the organification of iodide. Food and Drug Administration issued a black box warning for propylthiouracil because of its association with liver failure. The goal of management of hyperthyroidism in pregnancy is to maintain the free thyroxine or free thyroxine index in the high normal range using the lowest possible dosage of thioamides to minimize fetal exposure to thioamides. Hypothyroidism the classic signs and symptoms of hypothyroidism are fatigue, constipation, intolerance to cold, muscle cramps, hair loss, dry skin, prolonged relaxation phase of deep tendon reflexes, and carpal tunnel syndrome. However, at this time there are insufficient data characterizing perinatal risks of subclinical hypothyroidism or benefits of treatment, so routine testing is not recommended. Women with iodine-deficient hypothyroidism are at significant risk of having babies with congenital cretinism (growth failure, mental retardation, and other neuropsychologic deficits). Pregnancy-Related Complications Anemia the definition of anemia according to the Centers for Disease Control and Prevention is a hemoglobin (Hgb) or hematocrit (Hct) value less than the fifth percentile of the distribution of Hgb or Hct in a healthy reference population based on the stage of pregnancy. The two most common causes of anemia in 224 Guidelines for Perinatal Care pregnancy and the puerperium are iron deficiency and acute blood loss. Anemia may be classified according to the causative mechanism (decreased production, increased destruction, blood loss) or red blood cell morphology (microcytic, normocytic, macrocytic) or whether it is an inherited or acquired disorder. Iron deficiency anemia during pregnancy has been associated with an increased risk of low birth weight, preterm delivery, and perinatal mortality. Screening and Diagnosis All pregnant women should be screened for anemia during pregnancy. Measurements of serum hemoglobin (Hgb) concentration or hematocrit (Hct) are the primary screening tests for identifying anemia. Hemoglobin and Hct levels are lower in African American women compared with white women. Asymptomatic women who meet the criteria for anemia (Hct levels less than 33% in the first trimester and third trimester and less than 32% in the second trimester) should be evaluated. Antepartum Management the initial evaluation of pregnant women with mild to moderate anemia may include a medical history, physical examination, and red blood cell indices, serum iron levels, and ferritin levels. Using biochemical tests, iron deficiency anemia is defined by results of abnormal values for levels of serum ferritin, transferrin saturation, and levels of free erythrocyte protoporphyrin, along with low Hgb or Hct levels. Those with iron deficiency anemia should be treated with supplemental iron, in addition to prenatal vitamins. Failure to respond to iron therapy should prompt further investigation and may suggest an incorrect diagnosis, coexisting disease, malabsorption (sometimes caused by the use of Table 7-1. Intrapartum Management Iron supplementation decreases the prevalence of maternal anemia at delivery. Transfusions of red cells seldom are indicated unless hypovolemia from blood loss coexists or an operative delivery must be performed on a patient with anemia. Severe anemia with maternal Hgb levels less than 6 g/dL has been associated with abnormal fetal oxygenation, resulting in nonreassuring fetal heart rate patterns, reduced amniotic fluid volume, fetal cerebral vasodilatation, and fetal death. Thus, maternal transfusion should be considered for fetal indications in cases of severe anemia. Venous thromboembolism accounts for approximately 9% of all maternal deaths in the United States. Pregnant women have a fourfold to fivefold increased risk of thromboembolism compared with nonpregnant women. The most important individual risk factor for venous thromboembolism in pregnancy is a personal history of thrombosis. The next most important individual risk factor for venous thromboembolism in pregnancy is the presence of a thrombophilia (both acquired and inherited). Other risk factors for the development of pregnancy-associated venous thromboembolism include the physiologic changes that accompany pregnancy and childbirth, medical factors (such as obesity, hemoglobinopathies, hypertension, and smoking), and pregnancy complications (including operative delivery). Evaluation and Diagnosis Women with a history of thrombosis who have not had a complete evaluation of possible underlying etiologies should be tested for both antiphospholipid antibodies and for inherited thrombophilias. Medical records, including imaging studies, from any prior venous thromboembolic event may be helpful in evaluation. Antepartum Management Therapeutic anticoagulation is recommended for women with acute thromboembolism during the current pregnancy or those at high risk of venous thromboembolism, such as women with mechanical heart valves. Other candidates for either prophylactic or therapeutic anticoagulation during pregnancy include women with a history of thrombosis or those who are at significant risk of venous thromboembolism during pregnancy or the postpartum period, such as those with high-risk acquired or inherited thrombophilias. Guidelines recommend obtaining platelet counts when initiating therapeutic unfractionated heparin therapy in order to monitor for heparin-induced thrombocytopenia.

Flagyl 250 mg online
Despite a theoretical risk virus warning purchase flagyl on line, no increase in breast cancer incidence has been found to date among trans women on hormones. Risk factors should be assessed on a case-tocase basis and according to current evidence-based algorithms. In trans women who have had a vaginoplasty, the prostate can be palpated in the anterior neovaginal wall. It is therefore important to perform periodic visual inspection with a speculum, looking for genital warts, erosions, and other lesions. Trans men, past or current hormone use: fi Breast cancer: Annual chest wall/axillary exam; follow breast cancer practices as for natal females (not needed following chest reconstruction, but consider if only a reduction was performed). If oophorectomy is performed, it is important that hormone therapy be maintained to reduce the likelihood of osteoporosis. Follow standard national screening recommendations for other cancers, including anorectal, if possible. Providers should be aware that afer a gonadectomy, if a trans client stops hormones, there could be a risk of osteoporosis. Tere is some early evidence that trans women may have lower bone density before initiation of cross-sex hormones, possibly due to lower involvement in physical exercise (avoidance of exercise to prevent muscle mass). In countries where there are national guidelines for osteoporosis screening, providers should encourage trans clients to participate in such screening. In several locations, including Mumbai, Chennai, Bangalore, and Hyderabad, clinics engaged healthcare providers who were sensitive to the needs of trans clients, and provided hormone care, information about gender transition, laser (hair removal) services, and referrals for gender-affrming surgeries. It also reduces loss to follow-up because clients typically receive a diagnosis and treatment within a single visit. Tus, where resources allow, it is recommended that screening with laboratory testing and aetiological diagnosis be conducted for all sexually active clients. As of May 2015, only three case reports have appeared in the published literature of gonococcal infection of a neovagina. Cross-sex hormone use may reduce fertility; this may be permanent even if hormones are discontinued. Estrogen may have the efect of reducing libido, erectile function, and ejaculation in trans women. Special considerations for trans women: Neovaginal walls are usually skin, not mucosa; when it is mucosa, it is urethral or colon mucosa. Perform periodic visual inspections with a speculum to look for genital warts, erosions, and other lesions. It is important to also check for the presence of urethral discharge and ano-genital discharge (using an anoscope) and genital ulcers. No similar data exist for trans men in this region, and a few studies amongst trans men in the United States show generally low levels of infection (Herbst et al. Research in recent years has documented the lack of interconnectedness between these various intervention components and the resulting losses to follow-up. Tese losses are greater across the cascade for trans people than amongst the general population. They are exacerbated amongst trans subpopulations, including trans sex workers, drug users, and youth. In some places that serve a larger trans community, there could be assistants who are trans persons themselves. Tese assistants may help in the collection of personal data, provide general information about the functioning of the service, and motivate users to take advantage of certain interventions. Tese may include the following: fi Anal/vaginal intercourse without a condom, including receptive anal/vaginal intercourse for trans men fi Insertive/receptive anal intercourse for trans women fi Receptive neovaginal intercourse amongst trans women who have had sex reassignment/gender-afrming surgery fi Sharing of injection paraphernalia during drug or hormone use, or for sof tissue fller injections Counselling also should take into account that erratic hormone use can result in mood swings, masculinising hormones increase libido, and feminising hormones may impair erections and thus make condom use more difcult (Bockting et al. Trans women and men may feel at a disadvantage in negotiating sexual practices and prevention behaviours because they perceive a shortage of partners willing to enter into a committed relationship. The desire to conform to specifc cultural beliefs and practices around gender roles may also contribute to heightened sexual risk. Like other at-risk populations, research has shown that for trans women, unprotected sex is most likely with noncommercial primary partners (Nemoto et al. Programmes may also provide trainings for healthcare providers and assist clients to access social support services, when available, that may cover treatment-related costs. They may not be welcoming to trans participants and may be ill suited to provide for the specifc needs of trans men and women. Whenever possible, social support for trans people should be provided, either ofine or online, by trans peers (Bockting et al. Anxiety and depression, including suicidal ideation and attempts, are prevalent and are associated with stigma and discrimination (Bockting et al. Evidence and data on mental health can be found in Chapter 3: Right to Health (Section 3. A mental health assessment is crucial, with particular emphasis on how the trans client has coped with the social stigma attached to gender variance. It is essential that healthcare providers are alert to manifestations of suicidal ideation. The American Association of Suicidology provides a list of signs that a provider can use to assess risk for suicide. Signs of acute suicide risk include talk about or threats of killing oneself, looking for ways to commit the deed. In the presence of such signs, clients should immediately be referred to a mental health service; support from a suicide prevention task force or service should be sought. As with all clients, the primary care provider should screen for psychiatric illness. Depression is common, so providers should ask about persistent depressed mood, anhedonia, and suicidal ideation, and treat or refer those with clinical depression. Clients who have experienced trauma should be asked about symptoms of post-traumatic stress disorder as well as other anxiety disorders. Substance use may occur as a means of avoidance coping in clients with gender dysphoria and/or in stressful environments. Referrals for psychiatric management should be made to mental healthcare providers who have an understanding of trans issues. Questions should address frequency of use, types of substances, doses, route of administration, conditions in which the use is more likely to occur. If responses suggest zero to low risk of substance use, service providers should follow up by inquiring about intentions of future use and strategies to deal with peer pressure or external stressors. Brief interventions show efects in reducing harmful use; motivational counselling could also be efectively provided by peers. Evidence and data on alcohol and substance use and dependence in the region can be found in Section 3. In order to ensure standards are met, implemented, and maintained, monitoring and oversight are crucial. With trans clients, a provider can assess how the trans person has coped with stigma and discrimination encountered during their transition. The healthcare provider should pay particular attention to whether or not the client was gender-nonconforming in childhood and what stigma management strategies were employed. If indicated, the health provider can assist the client in identifying or adopting efective stigma management strategies. This may include providing information about complaints procedures, anti-discrimination bodies or peer support networks. The negative efects of abuse and violence need to be assessed, and referrals to counselling provided as needed.

