Duricef
Discount duricef 250 mg without prescription
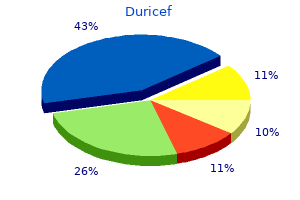
Patients frequently present with pain syndrome located in the neck-shoulder-arm region symptoms of pregnancy cheap duricef 500 mg fast delivery, which sometimes makes it difficult to differenti ate neck and shoulder problems. Before the diagnosis of non-specific neck pain 436 Section Degenerative Disorders can be made, it is mandatory to exclude differential diagnoses. General aspects of history-taking and physical examina tion are presented in Chapter 8. History Differentiate neck the predominant symptom for patients with degenerative cervical disorders is and arm pain pain. Key question How much of your pain is in your arm(s)/hand(s) and in your neck/shoulder(s) Cardinal symptoms of radiculopathy and myelopathy Radicular syndrome Myelopathic syndrome radicular pain numb, clumsy, painful hands sensory disturbances difficulty writing motor weakness disturbed fine motor skills reflex deficits difficulty walking symptoms of progressive tetraparesis (late) bowel and bladder dysfunction (late) the key finding in patients with a radicular syndrome is radicular pain,i. It is important to note that the pain not only radiates into the skin (dermatome) but also into the muscles (myotomes) and bone (sclerotomes)(seeChapter 8). Differentiation of radicular the referred type of pain is sometimes difficult to differentiate from non-spe and referred arm pain cific radiating pain, which is not caused by a nerve root compromise. The radicu is sometimes difficult lar pain can be preceded by neck pain which results from an incipient disc herni ation, i. The examiner should particularly ask for dis turbed fine motor skills (particularly writing skills). The pathoanatomical cause of the myelopathy characterizes the clinical presentation. Patients with cervical myelopathy can present with a broad spectrum of signs and symptoms. Cervical myelopathy is a clinical syndrome and dysfunction of the spinal cord, depending on the magnitude of spinal cord dysfunction and its chronicity. Early symptoms include diminished dexterity and subtle changes in balance and gait. Myelopathy can concomitantly appear with radiculopathy since central stenosis is often combined with foraminal stenosis. Spondylotic syndrome recurrent episodes of neck pain night and early morning pain pain aggravation with motion vegetative symptoms position dependent neck pain vertigo and dizziness non-radicular arm and shoulder pain headaches the spondylotic syndrome is more difficult to describe than a radicular and myelopathic syndrome. The pain arises from painful motion segment degenera tion and can be attributed to different pathoanatomical alterations, i. We therefore prefer to generally summarize the neck pain resulting from the degenerative motion segment as spondylotic pain. Vegetative symptoms and Patients often report vague numbness, thermal sensations, and tingling. The vertigo are not uncommon causes of vertigo and dizziness are not well explored [39, 90]. Some of these vege tative symptoms are caused by disturbance of sympathetic nerves which richly innervate the cervical spine [152, 308]. Headaches are frequent concomitant symptoms [118] and sometimes pose a difficult differential diagnosis. Physical Findings Even if the patient presents only with shoulder arm pain, a thorough examination of the whole spine is recommended. In patients with radiculopathy, frequent findings are [272]: sensory deficit motor deficit reflex deficits positive Spurling test positive shoulder abduction or depression test positive axial traction test the Spurling test or neck compression test is performed with the patient in the Provocation tests sitting position (see Chapter 8) [272]. The neck is extended and rotated to the are helpful in diagnosing side of the pain. Then, a careful axial compression of the head is applied; if posi radiculopathy tive, the patient reports pain radiating along the compromised nerve root [75]. In patients with cervical myelopathy, frequent findings are [68, 172, 238]: atrophy of the interosseous muscles gait disturbances and ataxia spasticity, hyperreflexia, and clonus pathologic reflexes, positive Babinski sign sensory and vibratory deficits muscle weakness positive Lhermitte sign the myelopathic gait Cervical spondylotic myelopathy is a combination of symptoms resulting from is broad, abrupt and jerky an impairment of segmental neural compromise and long tracts. The segmental compromise includes sensorimotor deficits consistent with a radicular deficit. Early symptoms are numb, clumsy hands and later atrophy of the interosseous muscles. In this context, a loss of power of adduction and extension of the ulnar two or three fingers and an inabil ity to grip and release rapidly with these fingers can be observed [198]. These patients have decreased vibratory and positional sense, and diminished fine motions in the hands. The gait disturbance manifests as spasticity and paretic dysfunction of the lower extremities. Additional symptoms are loss of balance, unsteadiness, stiffnesswithambulation,andcomplaintsoflossofpowerinthelowerextremi ties. The myelopathic gait is broad based with abrupt motion sometimes more hesitant and jerky. Gait is assessed by asking the patient to walk on the line and walk with closed eyes. Sensory changes vary widely according to the location and extent of the spinal cord dysfunction. Upper motor neuron findings such as spasticity, clonus and hyperreflexia may be present in upper and lower extremities. Long tract signs such as Babinski, Oppen heimer and Gordon as well as persistent clonus are indicative of upper motor neu ron lesion. Sensory disturbances in cervical myelopathy include loss of pain and temperature, proprioception, and vibration below the level of the lesion, whereas touch is often preserved [57]. Altered vibratory sense and proprioceptive changes are often present in cases with chronic or severe myelopathy. In a study of 55 patients with cervical spondylo tic myelopathy, Gregorius et al. In patients with spondylotic syndrome, findings are: stiff neck with limited range of cervical motion neck pain on extension and rotation referred pain on motion (occiput, shoulder, upper limb) chronic trapezius myalgia Degenerative Disorders of the Cervical Spine Chapter 17 439 Functional Assessment One of the first outcome assessments of cervical spinal disorders was proposed A standardized functional by Odom and is still frequently used [193]. However, there is a con to assess outcome sensusthatsuchacrudeoutcomeassessmentisinsufficientandnotpatient based [36]. It is therefore recommended to use self-rating scales such as the Neck Pain and Disability Questionnaire [285] and the Neck Disability Index [275] (Chapter 40). The grading system involves six grades (0 to 5) with progressive disability for ambulation (not affected to chair bound/bedridden). However, the application of this score for non-Asian patients is limited by the fact that one assessment considers the use of chopsticks. Diagnostic Work-up A thorough history and physical examination allow the diagnosis of radiculopa thy and myelopathy in the vast majority of cases. In this regard, imaging studies are helpful in identifying the correct level of neural compromise. On the con the causes of neck pain trary, the diagnostic work-up for neck pain remains challenging because degen are not well defined erative alterations are frequent in asymptomatic individuals [29, 215]. The corre lation of structural alterations to neck pain often requires further investigation. Even with spinal injections, the sources of axial neck pain cannot be identified with certainty. Standard Radiographs Standard radiographs of the cervical spine in the anteroposterior and lateral planes demonstrate: sagittal profile.
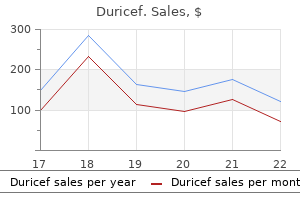
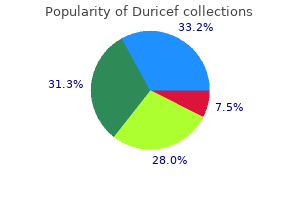
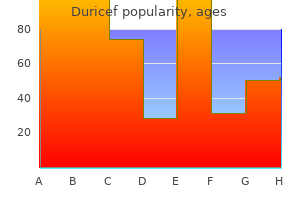
Buy cheap duricef 500mg on-line
Over the past several days she has become more short of breath symptoms pink eye order 250mg duricef visa, and this has considerably worsened over the past several hours. Physical examination shows marked jugular venous distention and bilateral rales to the apices. The electrocardiogram shows signs of an old anterior wall myocardial infarction, and the chest x-ray is consistent with a dilated cardiomyopathy and poor left ventricular function. Ischemia, arrhythmia, infarction, noncompliance with medications or diet, insufficient medications, or infection can all precipitate acute left ventricular dysfunction in this patient. This is why normally benign rhythms like atrial fibrillation can result in pulmonary edema. Because the problem comes from too much fluid in the lungs, the treatment is based on reducing this by: Diuresis, as rapidly as possible to decrease preload; furosemide is given in double doses every 20 min until sufficient urine is produced Morphine, which dilates pulmonary vasculature and also decreases preload Nitrates, which dilate the venous system and reduce blood return to the lungs Positive inotropes, which are useful only for impaired left ventricular function. We know that it can be characterized by disseminated intravascular coagulation, fibrinoid necrosis of arteriolar walls, microangiopathic hemolytic anemia, and dilation of cerebral blood vessels, but the root cause is unknown. About 1% of patients with hypertension will develop a hypertensive crisis at some point, and very rarely is it the first manifestation of hypertensive disease. Cocaine-induced hypertensive crisis is treated with the alpha blocker phentolamine. The day before she came in, she had been jogging around the school track and suddenly passed out. She reports regular menses since age 12 and has noted no association between the syncopal episodes and her menstrual cycle. Cardiovascular examination shows prominent apical impulse, S4 gallop, and a 2/6 systolic murmur at the lower left sternal border. In this patient, the prominent findings on physical examination point to a cardiac etiology. Characteristic findings on physical exam include sustained left ventricular apical impulse, prominent S4 gallop, and harsh systolic ejection murmur, loudest at the left lower sternal border and often associated with a thrill. Valsalva maneuver results in augmentation of the murmur, whereas squatting diminishes it. Further Management Plan Echocardiogram Troponin Test Results Thickened ventricular septum, which is hypertrophied disproportionately to the posterior wall of the left ventricle. Life-threatening arrhythmias, myocardial ischemia, and sudden death are all complications. They all help reduce the left ventricular-chamber size and therefore worsen the obstruction. Although she has been symptomatic for several months, she now comes at the insistence of her employer because she is starting to cough up blood on a regular basis. The patient is young for aortic stenosis, 162 and the cardiac exam does not support this form of lesion in which you would expect to find a systolic murmur at the right second intercostal space. The symptoms imply that the stenosis is becoming severe, but only cardiac catheterization from the arterial side can give a precise estimate. Mechanism of hemoptysis: pulmonary hypertension Mechanism of atrial fibrillation: dilation of left atrium Mechanism of opening snap: mitral valve leaflets suddenly stopping Basic Science Correlate Rheumatic fever causes fibrosis of the mitral valve. If the rate is not sufficiently controlled with digoxin, a small dose of a beta-blocker is useful. Surgical therapy should be implemented before the onset of pulmonary hypertension. When he stops, the pain goes away, and then it begins again if he continues another 3 blocks. Right leg has diminished femoral pulse compared with the left, and there are no popliteal or pedal pulses palpable. He has a history of myocardial infarction, which already indicates arterial disease, and he is a long-term smoker. Atrophic changes such as diminished peripheral pulses on the side of the pain and the absence of hair with smooth, shiny skin also contribute to the diagnosis. The femoral and popliteal arteries are the most commonly involved in artherosclerosis of the extremities. If the clinical situation deteriorates, however, to the point where the patient develops rest pain or becomes incapacitated (to the point of not being able to function), then arteriography and consideration for surgical revascularization will be necessary. It is useful only for planning surgical bypass or angioplasty by helping to determine the exact site of the lesion. Cilostazol is an agent used in peripheral arterial disease: Both a vasodilator and an antiplatelet agent Has been shown significant effects in prolonging exercise tolerance and for decreasing symptoms Is clearly superior to pentoxifylline (there is no clear benefit of pentoxifylline) In the past there has been concern about the use of beta blockers in those with peripheral arterial disease. Physical examination reveals chest contusions visible over the sternum and several tender ribs. The compression of the heart will cause decreased cardiac output and the backup of blood into the neck veins. Diuretics should not be given because they decrease right ventricular filling pressure and can make the collapse of the right side of the heart even worse. He was getting up from a seated position and started to play with his grandson when he suddenly lost consciousness. Pulmonary exam shows minimal breath sounds, and faint expiratory wheezes are heard throughout with prolonged expiratory phase. Examination of the abdomen is normal, and examination of extremities shows no thigh swelling or edema. In a young patient presenting with shortness of breath with an underlying pulmonary disease such as asthma, a secondary pneumothorax needs to be considered. Nebulizer treatment with short-acting beta-agonist-2 agonists (first-line bronchodilator) and can add nebulized short acting anti-cholinergics 182 2. Discussion Asthma is a disease characterized by inflammatory hyperreactivity of the respiratory tree to various stimuli, resulting in reversible airway obstruction. The combination of mucosal inflammation, bronchial musculature constriction, and excessive secretion of viscous mucus causing mucous plugs produces bronchial obstruction. Extrinsic (allergic) asthma (20% of cases) results from sensitization and is precipitated by allergens. The typical aspirin sensitivity affecting adults (10%) is nasal polyposis syndrome, which usually starts with perennial vasomotor rhinitis; later, asthma appears that occurs with minimal ingestion of aspirin. In a mild attack, slight tachypnea, tachycardia, prolonged expirations, and mild, diffuse wheezing is seen. In a severe attack, the use of accessory muscles of respiration, diminished breath sounds, loud wheezing and intercostal retraction are seen. Patients with poor perception of increasing asthma symptoms may also benefit from assessment of their peak expiratory flow rate at home. For mild intermittent asthma, recommend a short-acting inhaled beta-2-selective adrenergic agonist. For mild persistent asthma, recommend inhaled glucocorticoids as initial long-term controller therapy, along with short-acting inhaled beta-2 agonists as needed. The mechanisms causing airflow limitation include contraction of airway smooth muscle, thickening of the airway wall due to inflammation and edema, and plugging of airways with mucus. The main component of the rapid changes in airflow limitation is the smooth muscle, and is the basis for beta-agonist therapy that directly relaxes smooth muscle.
Generic duricef 500 mg overnight delivery
Furthermore medications excessive sweating discount duricef 500 mg visa, pain however, when concurrent interventions were taken relief of 50% or greater was achieved only in the tri into consideration. Considering that no con They showed an incidence of 58% prevalence of facet trolled diagnostic blocks were used, and no mention joint pain based on inclusion criteria of phase 1 of their was made of at least an 80% relief of pain following a study. Failure to exclude placebo responders may have diagnostic block, this study was excluded from the final diluted the findings of true responses, making detec evaluation. Pain Relief and Study Results Function Study Outcome Short Long-Term Characteristics Participants Interventions Comments Measures 3 6 12 term Methodological > 6 12 mos. Most problems, such as local observational studies (1391-1395), the evidence for swelling, pain at the site of the needle insertion, and intraarticular injections is limited. The most common complications of lumbar facet the pharmacology of the steroids (875). The major joint interventions are twofold: complications related to theoretical complications of corticosteroid administra the placement of the needle and complications related tion include suppression of the pituitary-adrenal axis, S130 Study Participants Interventions Outcome Pain Relief and Function Results Comment(s) Measures 3 mos 6 mos 12 mos Short Long-Term Study term Characteristics > 6 12 6 mos mos. Based on the pres A study by Manchikanti et al (282) included over ent evidence, there is good evidence for conventional 7,500 episodes, or 43,000 spinal facet joint nerve blocks, radiofrequency neurotomy and fair to good evidence with 3,162 lumbar facet joint nerve blocks performed for lumbar facet joint nerve blocks for the treatment under fluoroscopic guidance in an ambulatory surgery of chronic lumbar facet joint pain both in short-term center by one of 3 physicians. However, the evidence is limited for tered during each procedure and postoperatively were intraarticular facet joint injections and pulsed radio prospectively evaluated. Multiple side effects and complications mended treatment is with radiofrequency neurotomy observed in lumbar facet joint nerve blocks included or therapeutic facet joint nerve blocks. Profuse bleeding, bruising, sore the sacroiliac joint is accepted as a potential ness, nerve root irritation, and all other effects, such as source of low back and/or buttock pain with or without vasovagal reactions, were observed in 1% or less. The sac Toxicity of local anesthetic with or without ste roiliac joint receives innervation from the lumbosacral roids has been extensively discussed (1430-1456). Neurophysiologi anesthetics relieve pain by inhibiting sensitization of cal studies have demonstrated both nociceptive and nerve endings (1430) and by reducing proinflamma proprioceptive afferent units in the sacroiliac joint tory cytokine production (1431-1433). Referral patterns based on sac anesthetics, bupivacaine has been one of the most com roiliac joint provocation and analgesic response to local monly used for injection therapy, and is considered one anesthetics in asymptomatic volunteers (1459) and pa of the safest drugs in terms of its potential for nerve tients with pain (1263,1483-1485) have been published. A number of in vitro studies have demonstrated a dose and time-dependent chon 3. In a systematic review evaluating a battery viability, studies have shown that bupivacaine may of tests to identify the disc, sacroiliac joint, or facet joint be toxic to intervertebral disc cells (1438-1441). Some as the source of low back pain, Hancock et al (375) sug (1442), but not all (1443), studies have demonstrated gested that a combination of sacroiliac joint pain pro synergistic toxic effects when steroids are combined vocative maneuvers appears to be useful in pinpointing with local anesthetic in vitro. The meta-analysis showed that the thigh loss of motor, proprioception, and sensory function; thrust test, the compression test, and 3 or more positive bowel and bladder dysfunction; Brown-Sequard syn stressing tests contain sufficient discriminative power drome; and spinal cord infarction. They Simopolous et al (17), in recent systematic review concluded that scintigraphy is at best of limited value in utilizing multiple studies and at least 50% relief as the establishing a diagnosis of ankylosing spondylitis. Radio positive rate of uncontrolled blocks of approximately graphic assessment, and history and physical examina 20%. They showed good evidence for diagnostic sac tion may only provide partial diagnostic information roiliac joint pain utilizing controlled comparative local (17,18,378,1462-1467,1471,1486-1536). The evidence was synthesized, modified from studies have established sacroiliac joints as a potential a systematic review by Simopoulos et al (17), based on source of low back and lower extremity pain (8,17,375, the relief criteria when sacroiliac joint injections were 377,378,401,403,1460,1461,1471,1472,1487,1537-1539). Based on the controlled diagnostic blocks, the sacroiliac Only one study (1493) was performed with a single joint has been implicated as the primary source of pain block with 50% to 74% pain relief; however, prevalence (8,17,375,401,403,1461,1463,1464,1471). The face validity of sacroiliac joint blocks has There were 2 studies evaluating 50% to 74% re been established by injecting small volumes of local lief with dual blocks (1489,1538). The prevalence rate anesthetic with contrast into the joint and determin in the 50% to 74% dual block category was 38% with ing contrast spread. When 50% relief joint blocks has been established by determining the with dual blocks was utilized as the criterion standard, false-positive rates of single, uncontrolled, sacroiliac the prevalence rate was shown to be 38% with a false joint injections of 20% to 54% (378,1488,1537,1538). Irwin et al (1538), in a large Positive responses may occur with extravasation of retrospective evaluation, found a prevalence rate of an anesthetic agent out of the joint due to defects 26. Negative results may oc There were a total of 8 studies meeting the inclu cur from faulty needle placement, intravascular sion criteria evaluating sacroiliac joint pain using a injection, or inability of the local anesthetic to reach cutoff threshold between 75% and 100% relief fol the painful portion of the joint due to loculations lowing a single block (377,388,1460,1487,1494,1495, (372,1461,1462,1466,1468-1470,1481,1490-1492). The prevalence in this group ranged from Hancock et al (375) suggested that a combination a low of 10% to a high of 62%. The 53% and 62% of sacroiliac joint pain provocative maneuvers appears prevalence rates reported by Dreyfuss et al (1487) to be useful in pinpointing the sacroiliac joints as the and Slipman et al (1494), respectively, were found in principal source of symptoms in patients with pain be highly selected populations. Slipman et al cluded that there is moderate evidence for the diagnos (1494) used 80% pain relief as the criterion standard, Overall, fying patients who might benefit from diagnostic injec a single block using 75% to 100% pain relief as the tions, they are not pathonomic (1263,1459,1483-1485). Using between 75% and 100% provocative tests may be useful to select patients for pain relief with dual blocks as the criterion standard has further study provided 3 or more of them are posi been advocated by some as the most rigorous means for tive. These include the distraction, compression, thigh diagnosing sacroiliac joint pain (8,712,1250,1341,1471). The In a small study that included only 20 patients, evidence is fair for provocative testing. Manchikanti et al (41) found a low prevalence rate of Based on numerous evaluations (388,398, 10%. In contrast, Laslett et al (1488) showed a preva 1289,1483,1494,1495,1500-1536,1539,1540), the evidence lence rate of 25. The for diagnostic accuracy of a painful sacroiliac joint with false-positive rate was 22% (378). Four systematic reviews have 38% with 50% to 74% relief with a dual block with only been conducted to evaluate the effectiveness of sac 2 studies available. Rupert et al (1461) evaluated the illustrated false-positive rates were similar with both role of intraarticular injections and radiofrequency types of dual blocks with 2 different criteria ranging neurotomy with inclusion criteria of a diagnosis of from 20% to 26% (Table 25). The evidence is fair ited evidence for intraarticular injections, conventional due to the limitation of the number of studies with 50% radiofrequency neurotomy, and pulsed radiofrequency to 74% relief with a dual block with only 2 studies avail neurotomy. A systematic evaluation of prevalence and diagnostic accuracy of sacroiliac joint interventions. Thus far, 4 systematic reviews have shown a lack of prolotherapy to steroid injections. The authors found significant evidence for intraarticular injections in man no significant differences at 3 months; however, on a aging chronic sacroiliac joint pain without spondyloar long-term basis, prolotherapy was more effective. However, in the recent assessment, Hansen a large retrospective study, Hawkins and Schofferman et al (18) showed emerging evidence for intraarticular (1499) reported positive results with intraarticular in injections, even though there are no well conducted jections performed appropriately under fluoroscopy. Borowsky and Fagen Our search criteria since the publication of the sys (1543) compared intraarticular injections with a combi tematic review showed no additional studies evaluating nation of intra and periarticular injections. In addition, Murakami et al (1546), performed evaluating intraarticular injections. The in a short-term follow-up, showed the superiority of characteristics of these studies are shown in Table 26. There is limited evidence for the effectiveness of Our literature search yielded no further studies. Our literature search identified one new study blockade of the ligaments and the neural supply. How comparing cooled radiofrequency neurotomy with con ever, the literature is scant in reference to periarticular ventional radiofrequency neurotomy (1551). The only systematic review assessing the role Cohen et al (1550) retrospectively evaluated 77 of periarticular injections is by Hansen et al (18) which patients with refractory, injection-confirmed sacroiliac showed poor evidence. Our search criteria yielded no joint pain who underwent sacroiliac joint denervation at other studies published since the publication of system 2 academic institutions. In multivariate analysis, preproce dure pain intensity, age older than 65 years, and pain 3. A trend was noted whereby patients receiving domized trials (1547-1549) and one observational study regular opioid therapy were more likely to experience (1543) as shown in Table 27. The use of cooled radiofrequency, the study by Lee et al (1547) was a randomized tri rather than conventional radiofrequency, was also asso al, whereas Borowsky and Fagen (1543) retrospectively ciated with a higher percentage of positive outcomes. In the ran were found to possibly influence outcomes, no single domized trial by Lee et al (1547), the authors showed clinical variable reliably predicted treatment results.
Order duricef 500mg overnight delivery
Larynx preservation with chemoradiotherapy (using laryngectomy for salvage) has been shown in randomised trials (42) (43) (44) (45) (46) (47) (48) (49) (50) to provide laryngeal preservation in the majority of cases without any detrimental effect on survival when compared with laryngectomy medicine 834 best duricef 250 mg. Therefore, it would be considered reasonable to offer radiotherapy to all patients with T3 laryngeal cancer and to reserve surgery for salvage. However, this is likely to be a small group and the majority of these will usually have locoregional symptoms requiring palliative radiotherapy. It may be possible in rare instances for a patient to have extensive M1 disease at diagnosis and not be recommended for radiotherapy. This would be a very small group and exclusion of these patients from the decision tree is unlikely to impact on the optimal radiotherapy utilisation estimate. Oropharynx There are no randomised trials addressing the treatment options (radiotherapy versus surgery) in oropharyngeal cancer. Therefore for the purposes of the decision tree, all oropharyngeal cancers are treated with radiotherapy. Radiation may be the preferred modality where the functional deficit will be great, and surgery may be the preferred modality where the functional deficit will be minimal. The results were identical in terms of relapse and survival between surgery and radiotherapy but the severe or fatal complication rate was substantially higher in the surgery group. The authors concluded that radiotherapy is the preferred primary treatment modality with surgical salvage reserved for persistent disease. Johns and Goldsmith (54) reviewed the literature and defined 4 groups of salivary gland tumours. The authors based their treatment of salivary gland malignancies on the size of the primary and the histopathologic diagnosis. Group 1 includes smaller tumours in the T1 and T2 classification with cell types that are associated with slow growth. T3 tumours and patients with nodal metastasis or recurrent tumours make up group 3. Radical parotidectomy with sacrifice of the facial nerve is usually required for a sufficient tumour-free margin in these patients, and postoperative radiotherapy is recommended. Group 4 includes T4 lesions and the extent of disease dictates excision and postoperative radiotherapy. Of all salivary gland tumours treated definitively, 81% were parotid, 18% submandibular, 1% sublingual. The remainder were high grade muco-epidermoid, adenocarcinoma, adenoid cystic, squamous cell carcinoma, malignant mixed or anaplastic tumours. Locoregional recurrence data for low-grade lesions treated with surgery alone were not reported. Local recurrence following surgery alone in the absence of adverse pathological features is reported by North et al. Surgical procedures included superficial (24%) or total (56%) parotidectomies and submandibular gland resection (20%). Since malignancy of the hypopharynx is generally clinically silent until the advanced stages, it is very unusual to diagnose these tumours at the T1 N0 stage. In addition, if the surgery of choice is pharyngolaryngectomy, then radiotherapy must be the preferred treatment to maintain function, using surgery for salvage. The proportion of these tumours that can be treated with conservative surgery alone would be so small as to make no significant difference to the overall utilisation rate. Therefore, all stages of hypopharynx cancer are recommended to have radiation for at least part of the treatment. The British Columbia group have not published guidelines for the management of paranasal sinus cancer. Accordingly in the decision tree, all non-metastatic nasopharyngeal carcinomas are designated to receive radiotherapy. The proportion of patients with M1 disease at diagnosis is small 5% in a series of 564 patients from Prince of Wales Hospital, Hong Kong (56), and 6% in 1555 patients with nasopharyngeal carcinoma treated at the National Taiwan University Hospital (57). A large proportion of these patients will however require radiotherapy for either locoregional symptoms or symptoms related to metastases to bone or brain. A small proportion of patients with liver and/or lung metastases will die from their disease without requiring radiotherapy. However, a detailed literature search failed to satisfactorily identify the proportion of patients that do not require radiotherapy. A study of all nasopharyngeal cancers treated in Finland 1980-1989 (58) revealed that 13/107 patients (12%) were treated palliatively due to age, severe co-morbidity or refusal to undergo radical radiotherapy. Metastatic squamous neck cancer with occult primary Indications for radiotherapy Most squamous carcinomas metastatic to lymph nodes of the upper half of the neck will originate from a head and neck primary site. However, in these patients the primary remains occult following standard head and neck examination and investigations. The indications for the use of radiotherapy either as definitive treatment or as an adjuvant to surgery for patients with metastatic squamous cell carcinoma of the head and neck where the primary is unidentified is controversial. The main intent is to not only maximise locoregional control in the neck but also to attempt to prevent the occult primary from becoming symptomatic. The Peter MacCallum Cancer Institute has developed treatment pathways for unknown primary squamous cell carcinoma of the head and neck (personal communication Prof. In their treatment pathway, routine radiotherapy either pre or post-operatively is recommended for >N2a disease and radiotherapy is considered optional for disease N1-2a. For the decision tree, the branch point for radiotherapy is for N1-2a not to receive radiotherapy. However, in the sensitivity analysis the branch point underwent modelling with the prevalence varying between the proportion with >N1 disease and > N2A disease receiving routine post operative radiotherapy to assess the impact that this variation has on the overall radiotherapy utilisation rate. From 1983-1992, 69 patients with unknown primary cancers of the head and neck were treated. All patients in this group maintained locoregional control (but the number of patients was very small). These data differs from that of Nguyen at al from the McGill University teaching hospital (36), who reported on 54 patients with metastatic squamous cell carcinoma to cervical lymph nodes. The decision tree uses the Sinnathamby rate of 9-22% of patients not receiving routine radiotherapy since this is the largest series and being Australian, this data is more likely to reflect incidence rates in other Australian treatment centres. The vast majority of N2a disease received radiation to the neck and head and neck mucosal sites. Recurrence or development of a symptomatic primary occurred in 54% of the N1-2 surgery alone group. None of the identified guidelines discuss the management of recurrent disease in this situation. However, it seems reasonable to assume that the vast majority of patients who develop recurrent disease would receive radiotherapy as part of their management, either alone for unresectable disease or post-operatively. Optimal Radiotherapy Utilisation Rate and Sensitivity Analysis Sensitivity analysis allows the assessment of the impact of varying the value of uncertain data items on the overall optimal radiotherapy utilisation rate. For the head and neck decision tree, 4 data items were identified as being uncertain. We therefore used incidence data to model between patients having radiotherapy for tumours > 4 cm in size as the smallest case scenario for radiotherapy (6% incidence) and >2 cm as the greatest case scenario for radiotherapy (25% incidence). To assess the impact of this uncertainty on the overall estimate of the need for radiotherapy in all head and neck cancers, a sensitivity analysis was performed for each of the variables. Once the decision trees for all tumours are completed, a tornado analysis will be performed whereby the impact of each of these variables on the overall estimate of the proportion of cancer patients needing radiotherapy will be examined. The graphs below show that the optimal proportion of head and neck cancer patients who should receive radiotherapy based on evidence is 78%. As head and neck cancer comprises 4% of all cancers, head and neck cancer patients suitable for radiotherapy represent 3. If early oral cancer were more routinely treated with radiotherapy then the utilisation rate would increase from 78% to 84%. This represents an increase in utilisation for head and neck cancer of 6% and an increase in the utilisation for all cancer by 0. Table 4: Optimal radiotherapy utilisation rates by head and neck sub type Tumour Sub-site % of head Overall optimal Proportion of all and neck radiotherapy cancer patients cancer utilisation rate that should for sub-site receive (%) radiotherapy (%) Oral Cavity 28 78 0. Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear and lip.
Order cheapest duricef
Pituitary gland treatment wpw generic duricef 250mg with amex, ovarian or breast recognizes a protein in melanocytes and melanomas. Specificity: this antibody recognizes an epitope on the Specicity: By immunohistochemistry, this an body specically extracellular domain of the gonadotropin releasing hormone recognizes a protein in melanocytes and melanomas. Intradermal nevi, normal adult melanocytes, and non-melanocytic cells are negative. Immunogen: Nuclei from pokeweed mitogen stimulated human Specicity: this monoclonal an body reacts with a protein of peripheral blood lymphocytes. Does not react with Bacteria, Helminths, and reacts very strongly with formalin-fixed, paraffin-embedded Spinach. Specicity: this monoclonal an body is specic to the heavy Posi ve Control: HeLa or HepG2 cells. Clone: H09 Specicity: this monoclonal an body is specic to the heavy Isotype: IgG2a chain of IgA and shows minimal cross-reaction with heavy chains Species Reactivity: Human of other immunoglobulins. It is reactive with all subclasses of Positive Control: Oligodendroglioma, diffuse astrocytoma Alpha heavy chain. It is reactive with all subclasses of Manufactured By: Dianova GmbH Alpha heavy chain. Specicity: Recognizes a protein of 75kDa, iden ed as gamma Specicity: Recognizes a protein of 75kDa, iden ed as the heavy chain of human immunoglobulins. It reacts with all sub-classes sub-classes of gamma chains of human immunoglobulins. It does not cross not cross-react with alpha (IgA), mu (IgM), epsilon (IgE), or delta react with alpha (IgA), mu (IgM), epsilon (IgE), or delta (IgD), (IgD), heavy chains, T-cells, monocytes, granulocytes, or heavy chains, T-cells, monocytes, granulocytes, or erythrocytes. It reacts with all Specicity: Recognizes a protein of 75kDa, iden ed as mu sub-classes of gamma chains of human immunoglobulins. It does not cross-react not cross-react with alpha (IgA), mu (IgM), epsilon (IgE), or delta with alpha (IgA), gamma (IgG), epsilon (IgE), or delta (IgD), heavy (IgD), heavy chains, T-cells, monocytes, granulocytes, or chains, T-cells, monocytes, granulocytes, or erythrocytes. Specicity: Recognizes a protein of 75kDa, iden ed as the mu Specicity: Recognizes a polypep de which is iden ed as heavy chain of human immunoglobulins. It does not cross-react insulin, a 51-amino acid polypeptide composed of A and B chains with alpha (IgA), gamma (IgG), epsilon (IgE), or delta (IgD) heavy connected through disulfide bonds. It does not cross-react Specicity: Recognizes a polypep de which is iden ed as with alpha (IgA), gamma (IgG), epsilon (IgE), or delta (IgD), heavy insulin, a 51-amino acid polypeptide composed of A and B chains chains, T-cells, monocytes, granulocytes, or erythrocytes. Localized to upper spinous and Specicity: Recognizes a polypep de which is iden ed as granular layers in normal skin. Localized to upper spinous and Immunogen: Puried human Ig kappa chain granular layers in normal skin. Isotype: IgG1, kappa Specicity: this monoclonal an body is specic to the kappa Species Reac vity: Human. Specicity: this an body recognizes a protein of 130kDa, Specicity: this an body recognizes a protein of 130kDa, identified as Ksp-cadherin. Specicity: this monoclonal an body is specic to the lambda Specicity: this monoclonal an body is specic to the lambda light chain of immunoglobulins and shows no cross-reaction with light chain of immunoglobulins and shows no cross-reaction with the kappa light chain or any of the five heavy chains. This antibody reacts with neutrophils, monocytes, reacts with neutrophils, monocytes, macrophages, and macrophages, and squamous mucosal epithelia and has been squamous mucosal epithelia, and has been shown to be an shown to be an important marker for identifying macrophages in important marker for identifying macrophages in tissue sections. Melanomas, gliomas, Species Reac vity: Human, Baboon, Monkey, Cow, Pig, Goat, neuroblastoma, non-small cell lung cancer, breast, gastric, Horse, Cat, Dog, Rabbit, Guinea pig, Rat, and Mouse. Specicity: Recognizes a protein of 42-46kDa, iden ed as Posi ve Control: Tonsil, lymph node, or spleen. Melanomas, gliomas, neuroblastoma, non-small cell lung cancer, breast, gastric, colorectal, ovarian, and renal cell carcinomas. Clone A103, M2-7C10 & M2-9E3 (Concentrate) Posi ve Control: Jurkat, Daudi, or HeLa cells. Detected at lower levels in bone marrow, thymus and Clone: A103, M2-7C10 & M2-9E3 lymph node, and at very low levels in colon and lung. This antibody labels melanomas and other tumors showing melanocytic differentiation. It does not stain tumor cells of epithelial, lymphoid, glial, or mesenchymal origin. It is also a useful positive-marker for melanomas and other tumors showing melanocytic angiomyolipomas. This antibody labels melanomas and other tumors showing melanocytic melanomas and other tumors showing melanocytic differentiation. Specificity: this antibody recognizes a 130kDa protein known as Specicity: this monoclonal an body recognizes a protein the Melanoma Cell Adhesion Molecule. This antibody labels Catalog Number Volume melanomas and other tumors showing melanocytic differentiation. Does not react with Mouse Isotype: IgG2b (M2-7C10 & M2-9E3); IgG2a (T311); IgG1 and Rat. Posi ve Control: Jurkat, A-431, HeLa or 501 Mel human Specicity: this an body recognizes a 60kDa an gen associated melanoma cells or Melanoma. Specicity: this an body recognizes a 60kDa an gen associated Specicity: this an body recognizes a 60kDa an gen associated with the mitochondria in human cells. The dominant epitope of 139H2 has not yet been Posi ve Control: HeLa or HepG2 cells. In immunohistochemical assays, it superbly stains Specicity: this an body recognizes a 60kDa an gen associated routine formalin/paraffin carcinoma tissues. This antibody to gastric mucin superbly stains routine formalin/paraffin carcinoma tissues. Isotype: IgG1, kappa Specicity: Recognizes a single glycoprotein of 520kDa, Species Reac vity: Human. Its antigen appears to be restricted to M2 and pancreatic carcinoma and pre-cancerous changes vs. Specicity: Mucin 6 expression is highest in the stomach and Specicity: Recognizes a myeloid associated dieren a on gall bladder, with lower expression in the terminal ileum and antigen in the cytoplasm of mature granulocytes. Mucin 6 is a secretory mucin, located in the deeper mucosal folds of human gall bladder, and its expression is altered with increasing degrees of inflammation. Specicity: Recognizes a phosphor-protein of 45kDa, iden ed Specificity: this antibody recognizes a myeloid associated as MyoD1. This antibody to MyoD1 labels the nuclei of myoblasts in It shows no reactivity with any other cell type in human tissues. Skeletal muscle or Specicity: Recognizes a phosphor-protein of 45kDa, iden ed rhabdomyosarcoma. Specicity: An -myogenin labels the nuclei of myoblasts in this antibody to MyoD1 labels the nuclei of myoblasts in developing muscle tissue, and is expressed in tumor cell nuclei of developing muscle tissues. This antibody to MyoD1 labels the nuclei of myoblasts in Specicity: An -myogenin labels the nuclei of myoblasts in developing muscle tissues. Cerebral Cortex Specificity: this antibody is specific for a pepsin-like aspartic Specificity: Recognizes a protein of ~140kDa, identified as N proteinase identified as Napsin A. Neuromas, ganglioneuromas, gangliogliomas, Species Reac vity: Human, Rat, Pig, Cow and Chicken. Anti-neurofilament the skin, and oat cell carcinomas of the lung also express stains a number of neural, neuroendocrine, and endocrine neurofilament. Soma and stains a number of neural, neuroendocrine, and endocrine axons of sensory neurons, and ganglionic satellite cells. Does not Posi ve Control: Neuronal axons, Schwann cells, and perineural react with Mouse and Rat. Soma and cells of peripheral nerves, or tumors of nerve sheath axons of sensory neurons, and ganglionic satellite cells. It is highly specific to in cell or tissue preparations and can be used as a marker of the p21 and shows no cross-reaction with other closely related nucleoli in subcellular fractions. This antibody is highly specific to p21 and shows no cross Posi ve Control: Epithelial cells in normal placenta or prostate reaction with other closely related mitotic inhibitors. F6 Isotype: IgG2a, kappa Isotype: IgG1, kappa Species Reactivity: Human, does not react with mouse and rat. It is highly specific to Specicity: this an body recognizes a 27kDa protein, iden ed p21 and shows no cross-reaction with other closely related as p27Kip1, a cell cycle regulatory mitotic inhibitor.
Order 250 mg duricef free shipping
For example symptoms endometriosis buy cheapest duricef, periventricular nodular heterotopia is associated with both epilepsy and dyslexia. Aberrant cortical to cortical white matter integrity has been found to be correlated with poor reading fluency8 whilst abnormal connections between the heterotopia and overlying cortex was related to longer seizure duration9. However, extratemporal cortical structural abnormalities in frontal, parietal and occipital cortex are reported as well as in subcortical and cerebellar regions with cognitive deficits extending beyond memory and incorporating executive function10,11. Age related brain development and atrophy contribute to the cognitive vulnerability in epilepsy. In healthy children, grey matter volumes decline with concomitant white matter volume increases12. However, children with epilepsy often exhibit abnormalities in brain structure at or near the time of seizure onset and an altered development trajectory early in the course of epilepsy13. However, it remains uncertain as to what degree of altered brain development is causal to cognitive abnormities and whether these changes are permanent upon remission of seizures and cessation of treatment. Dynamic mapping of human cortical 15 development during childhood through early adulthood. Patients with epilepsy have a lower baseline cognitive reserve circuitry and executive dysfunction in recent-onset juvenile myoclonic epilepsy. Neuropathology of the blood-brain barrier and pharmaco-resistance in human epilepsy. Neurofibrillary tangle pathology and Braak staging in chronic epilepsy in relation to traumatic brain injury and hippocampal sclerosis: a post-mortem study. Chronic temporal lobe epilepsy: a neurodevelopmental or progressivelydementing disease Cognitive prognosis in chronic paroxysmal depolarizations of neurons producing a rapid succession of action potentials lasting temporal lobe epilepsy. Enhanced oscillatory activity in the hippocampal-prefrontal network is related to short-term memory function after early-life seizures. For example, in rats exposed to early life seizures, impairments in hippocampal-dependent tasks are noted in adulthood. Cognitive rehabilitation in adults including simple external aids such as diaries, calendars or computer-assisted apps along with online or face 2 face self-management programmes can be helpful, although the evidence for consistent and sustained benefit is mixed. Language in benign childhood epilepsy with centro-temporal spikes abbreviated form: rolandic epilepsy and language. Neuropsychological profile of patients with juvenile myoclonic epilepsy: a controlled study of 50 patients. A structural basis for reading fluency: white matter defects in a genetic brain malformation. Neurodevelopmental vulnerability of the corpus callosum to childhood onset localization-related epilepsy. Following this, editorials and reviews have been published on a regular basis, all highlighting what was hitherto a lack of familiarity with the current literature and urgent need for evidence-based guidelines. There seems now to be little doubt that epilepsy patients are at increased risk of fractures and metabolic bone disease, to an extent that we should be at least discussing with our patients. But many issues remain unresolved, including which of the multiple mechanisms are most important, whether newer drugs offer advantages over older drugs, how best we should identify those most at risk, and what preventive treatment should be offered. This chapter reviews the currently available literature and discusses recommendations based on this. Definitions and assessment the primary symptom of metabolic bone disease is an increased incidence of fracture. There is considerable individual variability, of which 80% is due to hereditary factors including sex and ethnicity (Caucasian women have the highest incidence of osteopenia, with Afro-Americans relatively protected)8. Serum levels of 25-hydroxy vitamin D are usually measured, and the lower limit of normal is now 30nmol/L, but a recommendation that in individuals with other risk factors, including those on antiepileptic drugs, a level of at least 50nmol/L should be maintained. Thus, populations who are housebound/institutionalised, or those who avoid sunlight for cultural reasons, will by default rely more on dietary sources and will be at risk of deficiency. Intestinal, liver, renal or cardiopulmonary diseases are also risk factors due to secondary effects. Importantly, many of these did not have known risk factors and thus would have been missed without screening. The bone isoform of serum alkaline phosphatase is the most commonly measured but is relatively insensitive as a screening test. There are several serum markers of bone formation, including osteocalcin (a non-collagenous matrix protein secreted by osteoblasts) and circulating peptides of type I collagen. Similarly, serum levels of peptides representing degraded products from osteoclastic activity. Bone turnover is increased during growth periods and fracture repair and such markers have been correlated with histology from bone biopsy in both health and disease16. Further research is required before they can be used to detect at-risk individuals or monitor treatment, so they will not be discussed here. Values can be obtained for whole bones or joints, or bone cortex or trabecular bone alone. Values taken from sites of potential fracture, ideally the total hip There are many reasons why patients with epilepsy might be at increased risk of bone disease, including score, are considered the most valid. The spine is not suitable for diagnostic purposes but can be used reduced exposure to sunlight (housebound/institutionalised), frequent falls, and lower physical activity to follow treatment effects. Results are usually expressed as T scores, representing the number of standard levels in patients with active epilepsy. It found the overall incidence of fractures to be doubled in epilepsy patients compared to age and sex matched controls. Although it has high specificity, the sensitivity is low (approximately 50%)12, 24,25 this was also the conclusion from recent meta-analysis studies, with the highest relative risks meaning that half of fractures will occur in patients said not to have osteoporosis on this measure. Others have reported that up to one-third of the increased risk21,26 appears to be a direct result Vitamin D metabolism of injury during seizures, again something supported by the meta-analysis24 and more recent studies27. The major biologically active metabolite of vitamin D is 1,25 dihydroxy vitamin D, which, in addition Thus optimum seizure control, especially where there are convulsive seizures and/or falls, remains to its roles in bone metabolism, has antiproliferative, prodifferentiation and immunosuppressive effects. Similarly, on biochemical markers of bone metabolism, offering a number of biologically plausible mechanisms in a recent population-based case-control study, the relative increase in fracture for patients on enzyme that might underlie increased fracture risk. It is also worryingly prevalent (40-80%) in epilepsy populations, both in the developed53 and though less markedly. Thus, whilst illustrating that there with enzyme inducers, is supported by meta-analysis studies25. This translates into up to an additional 48 fractures for every 10,000 women treated with non-validated methods/sites and are thus difficult to interpret. Biochemical markers Given the now huge number of available drugs/drug combinations, this is perhaps not surprising. Using Prior to the last twenty years or so, nearly all published data had been in the form of case reports, a surrogate marker of cumulative drug burden (the total duration of epilepsy multiplied by the number cross-sectional, or retrospective studies, and thus subject to potential biases. This Studies in children and adolescents are generally smaller, with an inevitably bigger spread of data reflecting may be exacerbated by additional effects on sex hormones2. Several well controlled earlier studies have not found any significant reduction gastrointestinal calcium absorption33. However, not all studies are consistent in terms of specific markers or individual drugs, and in terms of detail there are many conflicting results. Prospective studies assessing bone health markers in relation to antiepileptic drug exposure. Despite feasibility and cost of any intervention are especially crucial and, as yet, largely not established. These ask for basic of the message across different studies using different methodologies suggests this is a real association.
Duricef 500mg on-line
In Western industrialized countries medicine games buy duricef line, patients today present with less specific symptoms and often have an underlying general illness. The prevailing symptoms in a study by Fam and Rubenstein were back pain and weight loss [13]. Diagnostic Work-up the most important aspect of diagnosing spinal infection is to include this diag Key to diagnosis is nosis in the differential diagnosis. The Infection parameters are parameters can reliably be used to monitor treatment response. The white blood sensitive but not specific cell count is only elevated in about half of the patients and depends on the nutri tional state of the patient. The determination of antibody titers for putative bac teria is valuable in identifying certain causative organisms. In the presence of a septic state, blood cultures should be obtained, but the hit rate is low. It can be increased if more than one blood sample (three to five recom mended) is taken from different veins. Inputativetuberculosis,theMantouxortuberculinskintestishelpfulto investigate present or past exposure to Mycobacterium tuberculosis. Radiographic findings in spinal infection the classical radiographic signs of spinal infection consist of a loss of vertebral endplate definition, b decrease of disc height, gradual development of osteolysis, development of a paravertebral soft tissue mass, and reactive changes with sclerosis. Imaging Studies Modern imaging modalities have substantially improved accuracy in diagnosing spinal infection. However, standard radiographs are still very helpful because they allow an overview of the osseous destruction and resulting deformity. Standard Radiographs Radiographic diagnosis is the major drawback of standard radiography is the delay in the appearance of hampered by a delay in the radiographic signs (Fig. Contrast enhancement is helpful in differentiating spinal tuberculosis Contrast enhancement from other granulomatous infections [46]. The key findings include paraspinal soft-tissue masses, vertebral destruction and collapse, epidural abscess, posterior element involve ment, and intraosseous abscess. However, an indication for a making the diagnosis bone scan is still the search for a focus lesion. Confusion may arise with regard to the differential diagnosis of a degenerative endplate abnormality and spinal infections. This is particularly valid in areas that are difficult to access, such as the sacrum or sacroiliac joints and upper thoracic or cervical region [48]. Percutaneous needle biopsy provides a definitive diagnosis ranging from 57% to 92% [7, 34, 39] and depends on previous antibiotic treatment. Differentiation of tuberculosis from tumor may sometimes be difficult and a cul Tuberculosis can ture takes considerable time. In the clinical situation it is not possible to await the mimic tumor results from the culture and the diagnosis has to rely on the imaging findings. Non-operative Treatment In the absence of a life-threatening condition, treatment of spinal infections Do not start treatment should not be started without vigorous attempts to isolate the causative organ prior to isolation of the ism. It is mandatory to obtain the causative organism prior to antibiotic treat causative organism ment because of the substantially reduced likelihood of a secondary diagnosis (if possible) (Case Introduction). In the absence of a causative organism and progressing infection despite (non-specific) antibiotic treatment, high-dose broad-spectrum double or triple drug chemotherapy is often required. However, subsequent severe pharmacological side effects may limit the use of high-dose antibiotics and may result in a life-threatening situation if the infection is not controlled. General objectives of treatment eradicate the infection prevent or reverse a neurologic deficit prevent recurrence restore spinal stability relieve pain correct spinal deformity the choice of treatment is related to the chances of achieving the general objec Non-operative therapy tives of treatment with the respective therapy (Table 2). While radical debride is still the gold standard ment, internal fixation, and appropriate antibiotic treatment have become the for uncomplicated cases gold standard in the treatment of osteomyelitis of long bones, the mainstay for 1030 Section Tumors and Inflammation Table 3. Favorable indications for non-operative treatment single disc space infection (discitis) mobile patients with only moderate pain known causative organism absence of relevant neurologic deficit absence of gross bony destruction and instability rapid normalization of inflammation parameters the treatment of spinal infection is still non-operative (Table 3). However, the trend in the literature is to support more aggressive treatment of spinal infections even in situations where non-operative treatment can be successful. Depending on the resistance of the organism and the bone penetration of the respective antibiotic drug, administration by the oral route may be appropriate for the post-primary treatment. We strongly recom mend that the antibiotic treatment be discussed with an infection specialist to a c d e Case Study 1 A 70-year-old woman presented with an infected great toe and was treated with antibiotics for 3 weeks after a biopsy was taken. The biopsy revealed Proteus mirabilis and Pseudomonas aeruginosa as the responsible germs. Two months later the patient developed severe neck pain, which became worse with movement. The radiographic evaluation of the cervical spine demonstrated blurred endplates and somewhat narrowed disc space (a). This case exemplifies the notion that detection of a germ after previous antibiotic treatment is unlikely. In the absence of a neurologic deficit, severe pain or substantial deformity, non-operative treatment was successful. Infections of the Spine Chapter 36 1031 allow for the most specific (narrow) drug therapy with the least chances of phar macological side effects. After this period, chemotherapy should be continued with isoniazid and rifampin in the absence of resistance or side effects. There is still debate on the optimal duration of antituberculous chemotherapy required for complete recov ery. While a minimum of 12 months is favored by the majority of experts, no con vincing evidence can be derived from the literature [35]. While bedrest may be indicated for the initial treatment, early mobilization of Early ambulation the patient with an orthosis is recommended. The need for cast immobilization, is attempted including neck or thigh extension, has to be determined on an individual basis and depends on the location of the infection, general condition, and age of the patient. Follow-up imaging stud in monitoring healing ies should be done in the case of persistent symptoms and in the absence of of infection decreasing inflammation parameters. Indication for a change from non-operative to operative treatment is the per sistence of the infection despite adequate antibiotic treatment or in the presence of pharmacological side effects. A recent study has demon strated a favorable outcome by surgical treatment in this situation [8]. Operative Treatment General Principles Although the majority of cases with spinal infections can be successfully treated non-operatively, surgery may become necessary in about one-third of the patients (Table 4): Table 4. Less information is available from the literature with regard to the treatment of pyogenic infections. On the other hand, no evidence is presented that the spinal infection responds differently to radical debridement and bone grafting than to long bone osteomyelitis. No reports indicate that this approach is ill-advised in cases where conservative treatment does not result in rapid reso lution of the infection and recovery of the patient. Surgical Techniques the surgical approach is largely dependent on the extent and location of the infection, spinal destruction, neurologic deficits, health status, and comorbidity of the patient (Fig. Surgical treatment of spinal infections the key to the treatment of spinal infections is radical debridement of the infected spine. In cases of thoracolumbar spondylodiscitis, an accepted standard for the treatment of spinal infection today is posterior instrumentation, followed by anterior radical debridement. If a kyphotic deformity is present, a lordic prebent rod is first inserted and connected to the dis tal screws. With curets and pituitary forceps, the infected area is debrided to the bleeding bone. Percutaneous Debridement and Drainage In discitis with suspicion of abscess formation, percutaneous debridement and drainage is the preferred treatment [17, 18].

